Treatment of Chordomas

Treatment Options for Chordomas
Treatment options for chordoma include surgery, radiation therapy, and in rare cases, chemotherapy. The best treatment strategy depends on several factors, including the size, type, and location of the chordoma, and your overall health.
The decision-making process is often multidisciplinary, involving neurosurgeons, radiation oncologists, medical oncologists, and other specialists. While it can be overwhelming to meet with multiple professionals, know that they are all working with your best interests in mind.
In general, surgery is the mainstay of treatment and provides the best chance at improving survival rates. The aim of surgery is to remove as much of the tumor as possible, without causing damage to the surrounding brain, nerves, or blood vessels.
In many cases, complete removal is challenging due to the chordoma's tendency to invade nearby tissues. However, a skilled surgical team can make a significant difference in terms of reducing the likelihood of complications and maximizing safe tumor removal.
Radiotherapy is usually given after surgery to target any remaining tumor cells. Radiation treatment works by damaging the DNA inside of the tumor's cells. When the DNA in a cancer cell is damaged, its ability to divide and grow is impaired. Ultimately, the damaged cancer cells die or are prevented from multiplying. If the chordoma cannot be treated through surgery, radiotherapy becomes the main treatment method.
Chemotherapy involves injecting anti-cancer medications into a vein in your arm. Since its effectiveness is limited, It is usually given after treatment options have been exhausted, or along with surgery and radiotherapy in certain cases. Research is ongoing to find effective and safe chemotherapeutic agents for chordoma treatment.

Surgery for Skull Base Chordoma
Surgery is the treatment of choice for chordomas. The type of surgery depends on the size and the location of the tumor. Skull base tumors are usually treated by endoscopic transnasal approaches or open surgical approaches.
In an endoscopic transnasal approach, the surgeon operates a a long, thin, cylindrical camera called an endoscope along with other long instruments that will be inserted into your nose to reach the tumor. This surgical approach is less invasive than open surgery and generally results in fewer complications. Another advantage of an endoscopic approach is less visible scarring.
After surgery, your nose will be bandaged and you may remain in the hospital for a couple of days for observation. You may have some discomfort in the nose and throat for several days after endoscopic transnasal surgery. Avoid sneezing, blowing your nose, bending, lifting heavy weights, or coughing for a few weeks following the operation. Eating a high-fiber diet with many fruits and vegetables will prevent constipation and reduce complications such as cerebrospinal fluid leak.
When the chordoma cannot be reached through an endoscopic approach through the nose, an open surgical approach is advised. An incision is made in the scalp, and an opening is made in the skull in a procedure called a craniotomy. The brain is gently retracted with surgical instruments to reach and remove the tumor. The skull bone will be placed back and fixed with screws, and the scalp will be sutured back together. You may feel some pain and swelling at the surgical site. Any sutures are typically removed after 7–10 days.
Some of the potential complications that can occur during or following surgery are bleeding, infection, and injury to surrounding structures. Additional complications include:
- Visual disturbances
- Hormonal disturbances caused by damage to the pituitary gland
- Cerebrospinal fluid leak from the nose or the surgical site
- Recurrence of the chordoma
If you have any questions about the surgery and its risks and benefits, do not hesitate to ask a neurosurgeon experienced in treating chordomas.
Surgery for Sacral Chordoma
Sacral chordoma, also known as tailbone chordoma cancer, generally requires surgery to remove as much of the tumor as possible. The most commonly performed surgery is called a wide resection. In this procedure, the tumor and some healthy surrounding tissues are removed. This is done to remove as many tumor cells as possible. Sometimes, a sacrectomy procedure is recommended. Sacrectomy aims to remove the entire sacrum and is usually done in cases of very large or difficult-to-access tumors. Reconstruction of the sacrum is an option following sacrectomy.
After the surgery, you may experience pain and swelling at the surgical site – this is normal. You will be advised to stay in the hospital for a few days after the surgery. Stitches are removed around 10 days after surgery.
Some potential risks of sacral chordoma surgery, in addition to bleeding and infection, are related to damage to nerves that are involved in several functions, such as:
- Disturbances with bladder and bowel function
- Difficulty walking
- Sexual dysfunction
These complications occur rarely in an experienced neurosurgeon’s hands. Being aware of the risks and benefits of surgery will help you to make an informed decision about your treatment.
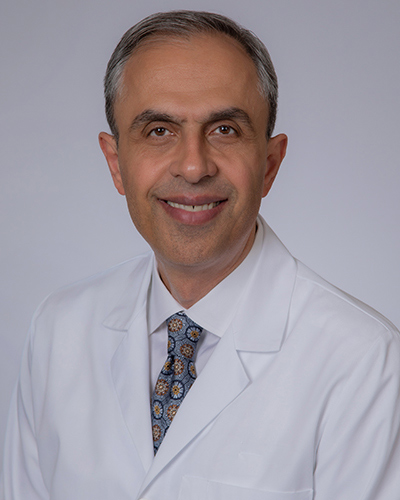
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Radiotherapy for Chordomas
Radiotherapy is a commonly used treatment for chordomas that involves targeting the tumor with high-energy radiation beams to inhibit the growth of tumor cells. They can be given from outside of the body (external beam radiotherapy) or from a radioactive source placed within or near the tumor (brachytherapy).
External beam radiation therapy is the most commonly used form of treatment, and is generally what comes to mind for most people when they think about radiation therapy. Radiation can be delivered via photon beams (e.g., X-rays) by a linear accelerator, or particle beams (e.g., protons) by a particle accelerator such as a cyclotron. Proton therapies offer the advantage of depositing the radiation dose more precisely on the tumor, and is generally reserved for tumors that are near critical structures such as the spinal cord or optic nerve.
When radiation is given after surgery, it is called adjuvant radiotherapy. When radiation is given before surgery, it is called neoadjuvant radiotherapy. While the aim of adjuvant radiotherapy is to treat remaining tumor cells, your doctors may recommend neoadjuvant radiotherapy to shrink the tumor down to a more manageable size for surgery. This can be important for particularly large tumors or those that are difficult to access surgically.
Radiation for chordoma treatment is typically administered in one session per day for 5 days per week, for 3 - 8 weeks. The exact treatment regimen may vary depending on your institution, machine, and beam type. Treatment is often given on an outpatient basis, meaning you should be able to go home after each session.
Like any treatment, radiotherapy can have potential side effects. These side effects can vary depending on where the treatment is being done, how much radiation is used, and the duration of treatment. Some side effects include feeling tired, changes in the skin (redness or dryness), feeling sick, losing hair, and possible infertility.
Before treatment, tell your doctor if you want to have children so other options can be considered. For some, memory problems can be a long-term side effect of radiotherapy. Side effects are different for everyone, and most of the time they can be managed.
Chemotherapy for Chordomas
Chemotherapy is a treatment that uses medications to destroy rapidly dividing cells. Doctors might use chemotherapy to slow the growth of chordoma after surgery or radiotherapy. The drugs are given to the patient through a vein in the arm in treatment cycles, with each cycle consisting of a period of treatment followed by a rest or recovery period. The number of cycles and how long they last will depend on your health and the type of chordoma.
As chemotherapy primarily targets rapidly dividing cells, it impacts not only cancerous tumors but also normal cells with similar characteristics, such as those in the skin, hair, and immune system. This can cause side effects, like feeling sick or tired, losing hair, and being susceptible to infections.
While it is uncommon, certain chemotherapy drugs have the potential to cause damage to the heart or lungs. Due to these potential side effects and limited effectiveness for chordoma, chemotherapy is typically not the first choice for this condition. Rather, doctors may use it along with surgery and radiotherapy. New drugs are currently undergoing testing for chordomas, potentially broadening the range of treatment options available.
Being diagnosed with a chordoma can be an emotional experience. Establishing a supportive circle of family, friends, and healthcare providers can help you to live a fulfilling life that is not defined by the chordoma. Familiarizing yourself with the various treatment strategies can help guide you through your chordoma journey.
Key Takeaways
- Chordomas are primarily treated with surgery, radiation therapy, and rarely chemotherapy
- Skull base chordomas can be treated either endoscopically through the nose or with open surgery through the scalp.
- Sacral chordoma surgery involves removal of the tumor and some surrounding healthy tissue.