The Recovery Outlook of Childhood-Onset Craniopharyngioma

In general, the outlook for patients diagnosed with craniopharyngioma is good and is improving. If the tumor can be mostly removed with surgery or a combination of surgery and radiation, there is an 80% to 90% probability of a potential cure. If the tumor reappears, it usually does so within the first 2 years after surgery.
Although survival rates are excellent, long-term hormonal, visual, and nervous system issues may arise after treatment. The disease may also recur if the tumor is not entirely removed. This article will discuss the recovery outlook of childhood-onset craniopharyngiomas in detail and the various factors that may influence it.
What Is a Craniopharyngioma?
A craniopharyngioma is a benign (non-malignant) tumor that develops slowly in the brain near the hypothalamus and pituitary gland. A developing tumor can place pressure on the pituitary gland, optic nerves, blood vessels, and brain tissue, causing symptoms such as:
- Problems with balance
- Confusion, mood instability, or changes in behavior
- Headache
- Increased thirst and urination
- Vomiting and nausea
- Slowed growth in children
- Vision problems
- Fatigue
- Appetite loss
- Weight changes
- Problems with learning and thinking
Craniopharyngiomas are sporadic tumors, which means they arise for no apparent reason and have no established risk factors. Researchers, however, believe they may result from a mutation in cells that make up sections of the pituitary gland in the developing fetus.
How Is Craniopharyngioma Diagnosed?
Following a comprehensive history and physical examination, the physician may request additional tests to assist in establishing the diagnosis. Some of these tests include imaging tests such as computed tomography (CT) and magnetic resonance imaging (MRI).
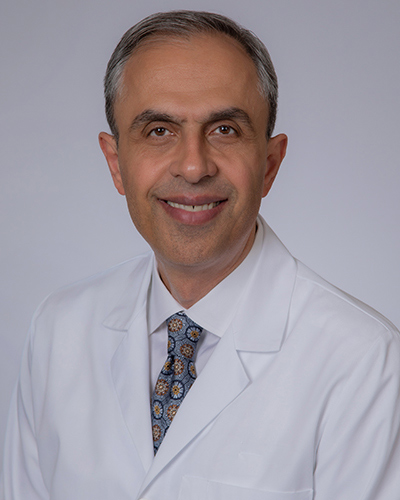
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Treatment Options for Craniopharyngioma
The 3 most common treatment options for craniopharyngioma include surgery, radiation therapy, and chemotherapy. The neurosurgeon and endocrinologist (a specialist in hormone disorders) will collaborate to create the best treatment strategy for the patient. Surgery and radiation therapy are the most often used forms of treatment for craniopharyngioma.
Recovery Outlook for Childhood-Onset Craniopharyngioma
The overall survival rate for childhood-onset craniopharyngioma has been increasing, with more long-term survivors. However, most children with craniopharyngioma do not return to full normalcy due to effects of the tumor and/or therapy. Long-term survivors of childhood-onset craniopharyngioma may need to cope with visual loss, thyroid disorders, hypothalamus dysfunction, and nervous system abnormalities.
In almost all cases of childhood craniopharyngioma, the pituitary gland does not make enough hormones (pituitary insufficiency). This can be treated by hormone supplementation medications. In detail, the recovery outlook of childhood craniopharyngioma may present as follows:
Visual Impairment
In around 50% to 80% of patients, visual acuity or visual field abnormalities persist over time. Visual difficulties are more likely in patients diagnosed with craniopharyngioma when they are younger than 10 years old.
Hormonal Challenges
Most long-term survivors of craniopharyngioma may have some degree of hormone insufficiency. Panhypopituitarism, defined as the lack of at least 3 pituitary hormones, has been reported in 75% to 95% of patients treated for craniopharyngioma during childhood.
Diabetes insipidus is also common; however, its severity varies depending on the type of treatment given. Diabetes insipidus is present in 70% to 90% of patients who have had surgical resection of a tumor attempted and in nearly all children who have had a tumor resection at less than 10 years of age. The incidence of diabetes insipidus is lower among children who received only intracystic chemotherapy.
Metabolic syndrome is a significant concern in individuals diagnosed with craniopharyngioma as children, with a greater incidence of high blood pressure, obesity, and type 2 diabetes. Adults with craniopharyngioma that began in childhood also face a higher risk of heart disease.
Quality of Life
Research on long-term quality of life after craniopharyngioma therapy observed that 30% to 50% of patients experience impairments in social function, school performance, and relationships. This may manifest with depression, withdrawal or social isolation, emotional outbursts, aggressiveness, and learning difficulties. It should be noted that caregivers may tend to report lower quality of life scores. In general, psychosocial aspects appear to be more affected than physical characteristics.
Mortality
Survivors of craniopharyngioma now have a much-improved life expectancy of up to 90% at 10 years. This means that 90% of patients go on to live at least 10 years or longer. However, craniopharyngiomas are linked to significant long-term morbidity primarily due to endocrine, hypothalamic, visual, neuropsychological, and cognitive side effects. This is attributed to the tumor itself or the potential side effects of treatment.
Increasing Chances for Improved Outlook
It is critical to think about craniopharyngioma as a long-term, or chronic, condition. Even if the tumor itself goes away, patients often must cope with impairments in functioning brought on by the tumor itself or its treatment. A supportive medical and caregiver team is essential to providing the best possible outcomes for the patient.
Complications During Treatment
Some of the complications that may arise during treatment include:
- Eye problems due to damage to the optic tract
- Hormone imbalances due to pituitary stalk or hypothalamus injury
- Psychosocial challenges such as depression caused by these complications or neurochemical imbalances from hypothalamic injury
These complications can arise due to damage from the tumor placing pressure or invading surrounding structures. They may also occur as a result of treatment because surgical or radiotherapy techniques may need to remove surrounding structures to achieve total tumor removal.
Thus, the craniopharyngioma patient requires a multidisciplinary approach that includes eye care, hormone management, neurosurgery, and psychology. Besides caring for physical aspects of this condition, it is just as essential to address emotional and social concerns.
Hypothalamic injury is a key factor in poor postoperative prognosis, obesity, and lower quality of life. In patients with a craniopharyngioma invading the hypothalamus, there will be an increased risk of hypothalamic dysfunction with surgical intervention, though what exactly that will entail can be unpredictable.
There is some evidence that 3D-modulated proton beam radiotherapy has the potential to target and minimize the radiation effects on optic and hypothalamic structures compared with conventional radiation techniques.
Clinicians face various obstacles when dealing with craniopharyngiomas, and the best therapeutic strategy for these rare tumors is still debated. Ultimately, the medical team will strive to craft a personalized treatment plan that aims to remove the tumor safely while minimizing damage to surrounding structures. Alternatively, if removal of surrounding structures is intended to achieve total tumor removal, the medical team must plan to treat other conditions that will arise with appropriate therapies.
Patients with craniopharyngioma have a higher post-treatment morbidity rate than the average population due to endocrine, hypothalamic, visual, and neuropsychological complications. Given the complexity of craniopharyngiomas, patients should be attended to by a multidisciplinary team of experts including neurosurgeons and endocrinologists to ensure the highest standard of care. Reach out to us today for more information on craniopharyngiomas.
Key Takeaways
A quick recap of childhood-onset craniopharyngiomas:
- The outlook for craniopharyngiomas is generally good and is steadily getting better.
- Unfortunately, most children diagnosed with a craniopharyngioma below 10 years of age do not regain totally normal functioning.
- Craniopharyngioma survivors may have to live with several hormonal and neuropsychological challenges.
- The outlook for craniopharyngiomas is dependent on the necessary mode and intensity of treatment.