Medical Management and Observation of Ependymomas

Ependymomas are tumors that can form in the brain or spine. Although they can develop at any age, ependymomas are more common in children and young adults. Surgery is typically the primary treatment option, but other interventions such as chemotherapy may be considered in special cases. Alternatively, a “wait-and-see” approach may be favorable for patients with low-grade and slow-growing tumors.
The use of chemotherapy for ependymoma is rare but may be recommended by your treatment team depending on your case. In this article, we discuss the various treatment options for ependymoma and focus on what medications are available, how they work, and their side effects.
Ependymoma Treatment Options
Treatment options for spinal and intracranial ependymoma fall into the categories of surgery, radiation therapy, and chemotherapy. Surgery is typically recommended first with the goal of complete removal of the ependymoma. If the tumor is in the brain, is a high-grade tumor, or if there are any residual tumor pieces remaining after the surgery, radiation therapy may follow. In some cases, a second surgery may also be considered if there is still evidence of a significant amount of tumor on imaging after the initial procedure.
Chemotherapy for Ependymoma
In certain cases, anti-cancer medicines (chemotherapy) may be used to treat the ependymoma. Currently, the role of chemotherapy in treating ependymoma is limited and reserved for infants or patients who have failed all other treatment options. Young children under 18 months old are typically treated with chemotherapy rather than radiotherapy because of their increased vulnerability to severe side effects and the potential long-term impact of radiation on cognitive functions.
Chemotherapeutic agents are often used in combination to prevent cancer drug resistance and because the synergistic effects of multiple drugs allow for lower doses and less toxicity. Certain medications are administered through a vein (intravenous or IV) or are taken by mouth. Some of the more common chemotherapeutic agents that may be used include:
- Etoposide
- Vincristine
- Cisplatin
- Cyclophosphamide
- Carboplatin
- Temozolomide
- Methotrexate
Chemotherapy is provided in cycles of treatment. One cycle of treatment is the time between the start of one round of chemotherapy and the start of the next one. For example, if you have 1 week of chemotherapy followed by a 3-week break without chemotherapy, this would be one cycle of treatment lasting 4 weeks.
The number of chemotherapy cycles can vary. Children with ependymoma may have 8 cycles of treatment lasting 8 weeks. This would mean chemotherapy treatments for approximately 1 year and 3 months.
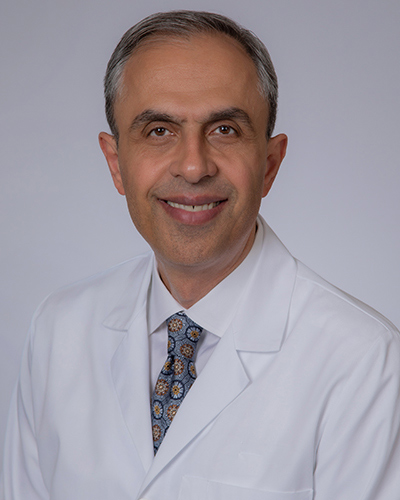
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
How Does Chemotherapy Work?
Chemotherapeutic agents generally work by inhibiting aspects of cell replication and causing cell death. These medications are particularly effective against rapidly dividing cells such as those present in the tumor. However, this means that they can also affect normal cells that are actively dividing, such as those on the skin, along the intestinal tract, or in the bone marrow. This can lead to side effects as described below.
Side Effects of Chemotherapy
Chemotherapy works best against rapidly dividing cells, but it is not specific to the tumor. Thus, common adverse effects of chemotherapy are related to its effect on other normal actively dividing cells such as those that make up our skin, hair, intestinal tract, and bone marrow. Common side effects can include the following:
- Nausea and vomiting
- Mouth pain or sores
- Abdominal pain
- Constipation
- Fatigue
- Hair loss
- Burning or tingling sensation in the hands and feet
The effect of chemotherapeutic medications on the bone marrow can cause decreased circulating levels of red blood cells, white blood cells, and platelets. Red blood cells carry oxygen from your lungs to your tissues, white blood cells protect you from infection, and platelets help you to stop bleeding. Loss of these cells can cause you to feel fatigued, get sick more easily, and bleed or bruise more frequently or more severely. During treatment, regular laboratory tests may be performed to monitor for severe chemotherapy side effects.
Ependymoma Response to Chemotherapy
The response of an ependymoma to chemotherapy can be hard to predict. Because the effectiveness of treatment is limited, chemotherapy is considered as a treatment option when all other options have been exhausted or if the patient cannot tolerate the side effects of other treatments.
Current research efforts are underway to investigate the role of chemotherapy in addition to surgery and radiation therapy, and the efficacy of new chemotherapeutic agents and targeted therapies. Clinical trials provide an opportunity to access these experimental treatments, but participation also involves potential risks that are not fully known.
Speak with your medical team about possible clinical trials that you or your child may be eligible to participate in. You can also search for ongoing ependymoma trials on ClinicalTrials.gov. Discuss the potential risks and benefits with your treatment team.
Observation for Ependymoma
The wait-and-see approach is an alternative to active treatment for ependymoma. This involves regular monitoring through imaging tests like an MRI to detect any tumor growth. This approach may be favorable for older patients with low-grade (e.g., Grade 1) ependymomas who are not experiencing symptoms. Financial or other situational factors may also be a barrier to initiating active treatment, but it's important to remember that you can always change your mind and pursue treatment options later when you feel ready.
Regular communication with your healthcare team is important to determine the best course of action for managing your ependymoma based on your treatment goals and current situation. Although observation without active treatment can be a viable option, it does come with some risks, such as the potential for the tumor to grow between scheduled imaging tests and invade nearby structures. However, this risk is low for low-grade tumors, as they tend to grow slowly.
It's natural to feel anxious or stressed when adopting the wait-and-see approach, as it may feel like you are not actively managing your tumor. However, over time, consistent imaging results demonstrating the stability of your tumor size can help provide reassurance. If you have any concerns or questions about the wait-and-see approach, it's important to discuss them with your healthcare team to ensure you are making an informed decision about your treatment.
Key Takeaways
- Chemotherapy is typically reserved for patients who have exhausted all other treatment options or children younger than 18 months of age.
- Response to chemotherapy for ependymomas can be difficult to predict, but research is ongoing to clarify the role of chemotherapy in combination with other treatment options.
- Clinical trials provide an opportunity to access new experimental treatments but also involves potential unknown risks.
- An alternative “wait-and-see” approach may be favorable for older patients with low-grade tumors, but can cause mental stress and anxiety.