Medulloblastoma: What the Patient Needs to Know

If you or a loved one are diagnosed with cancer, it might take days or even weeks to begin accepting this new reality. In a young child, a cancer diagnosis can seem like an awful mistake. Unfortunately, tumors can appear in individuals across all ages. While cancer is usually associated with older adults, certain types of tumors are found more commonly in children.
Medulloblastoma is one of them. In this article, we provide a comprehensive overview of all aspects of this condition to help guide you through this medical journey. The sheer volume of information and terms from the many unfamiliar faces of your new medical team can be overwhelming. Take a moment to breathe and remember that you can revisit these pages at any time.
What Is Medulloblastoma?
Medulloblastoma, pronounced "med-joo-low-blast-oh-ma", is the most common type of cancerous (malignant) brain tumor in children, accounting for approximately 20 - 25% of cases. It is thought to arise from cell populations present during early development in or near the cerebellum.
The cerebellum is an important part of the brain located at the back of the skull. It controls balance, coordination, and complex motor functions. The presence of a medulloblastoma can cause problems in the cerebellum, leading to changes in how you move and perform everyday tasks.
The fourth ventricle is another structure located immediately in front of the cerebellum that is often involved. It is part of the ventricular system of the brain, a network of interconnected fluid-filled cavities (ventricles).
A clear, watery substance called cerebrospinal fluid (CSF)is continuously produced and flows through these spaces to provide cushioning for the brain, remove waste products, circulate nutrients and hormones, among other functions.
When a medulloblastoma becomes large, it can fill the fourth ventricle and block the flow of CSF. This can cause pressure to build up in the brain in a condition known as hydrocephalus.

Figure 1: Please note the location of the cerebellum in the back of the head.
What Are the Symptoms?
The symptoms of medulloblastoma can vary depending on the tumor's size, exact location, and whether it has spread. Common symptoms can include:
- Headache
- Nausea and vomiting
- Problems with balance and coordination
- Difficulty with fine motor skills
- Changes in behavior or personality
- Fatigue and lethargy
- Vision problems, such as double vision or blurred vision
- Difficulty walking or a change in the way the person walks
This can manifest in young children as an inability to walk, bumping into objects, frequent trips and falls, and persistent crying. In infants, symptoms might also include a rapidly increasing head size due to fluid buildup in the brain.
If the tumor spreads to the spinal cord, it can cause pain or weakness in the legs. It is important to see a doctor if any of these symptoms develop, especially if they persist or worsen.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
What Are the Causes?
Medulloblastoma, like any tumor, is caused by genetic mutations. However, why exactly these gene alterations occur is unclear. Although there are no known environmental risk factors, certain hereditary conditions can increase the risk of developing medulloblastoma, such as the ones listed below.
- Gorlin syndrome
- Rubinstein-Taybi syndrome
- Turcot syndrome
- Li-Fraumeni syndrome
This list is not all-inclusive. Other rare hereditary syndromes involving mutations in the genes responsible for repairing DNA damage can also be associated with medulloblastoma development.
How Common Is It?
Although medulloblastoma is the most common malignant brain tumor in children, it is still relatively rare with an overall incidence of approximately 2 cases per 1 million people. This rises to 6 cases per 1 million among children. The median age at diagnosis is typically around 9 years old. While most cases occur in children, a quarter of medulloblastomas appear in adults.
How Is It Diagnosed?
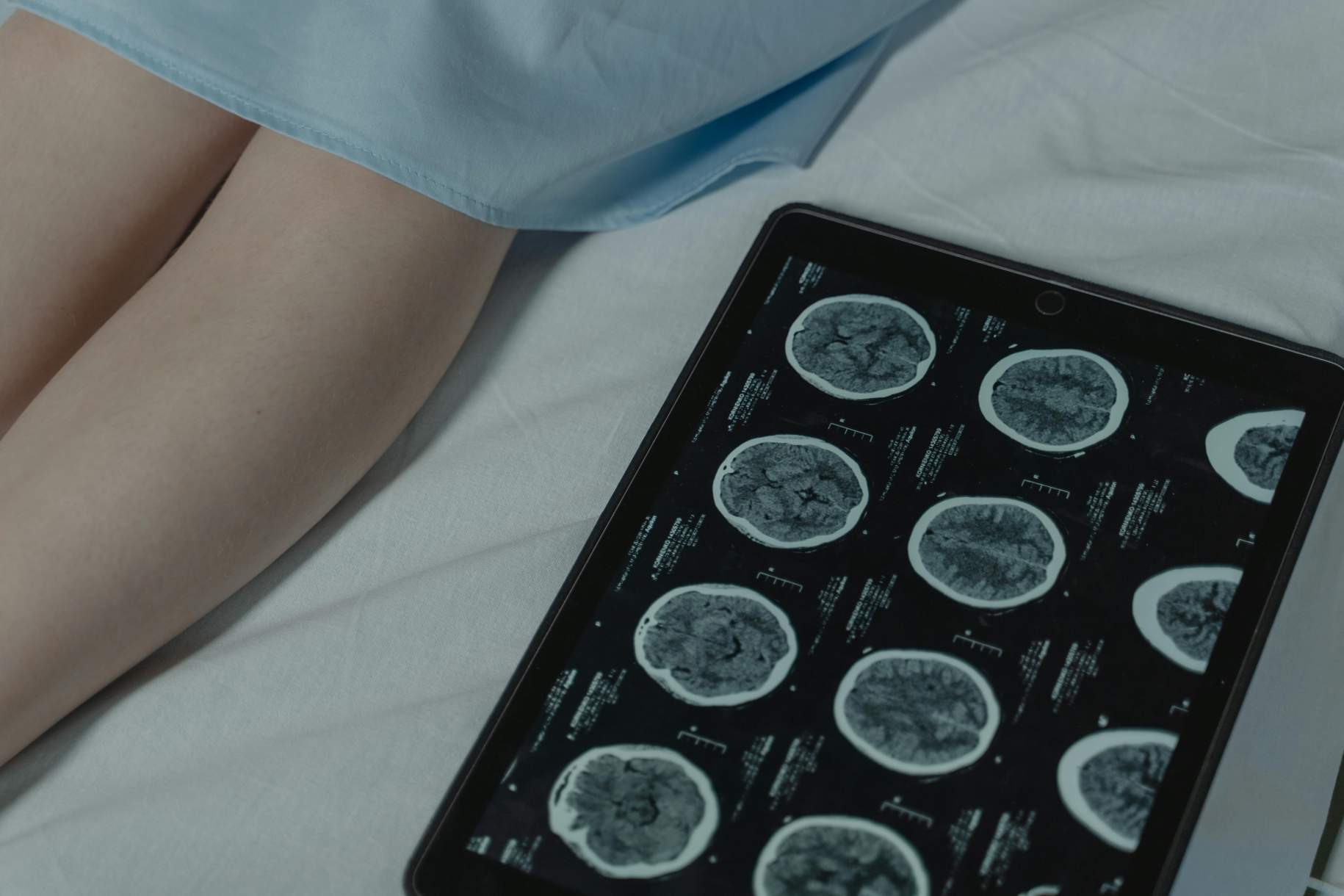
The diagnosis of medulloblastoma requires a series of imaging and molecular tests. Initially, a computed tomography (CT) scan may be ordered. This is a relatively quick test that can help to visualize structures within the head and determine whether an abnormal growth is present.
Oftentimes, a magnetic resonance imaging (MRI) scan is also obtained. This is another imaging test that provides much more detail than a CT scan. Although it takes longer to perform, no radiation is involved. The MRI will also be obtained for the spine to check for tumor spread.

Figure 2: Imaging tests demonstrate a contrast-enhancing mass in the fourth ventricle of the brain (top 4 images). Additionally, multiple nodules are noted in the brain and the spinal cord (bottom 2 images). This is indicative of an aggressive medulloblastoma with metastatic spread.
Additionally, a lumbar puncture can be performed to look for abnormal cells within the CSF. This can also help to assess for microscopic tumor spread that is too small to be detected on imaging.
Although an imaging test can help to locate an abnormality within the brain or spine, it cannot diagnose a medulloblastoma with absolute certainty. This is where a tissue biopsy comes in.
In a biopsy, the surgeon will remove pieces of tissue from this mass, then send it to another physician (pathologist) who will view the specimen under a microscope and perform additional tests to confirm the diagnosis.
These molecular tests are particularly important for categorizing the medulloblastoma into different types. Although all medulloblastomas are classified as World Health Organization (WHO) grade 4 tumors (the most aggressive type), survival and response to treatment can differ widely among the different types of medulloblastoma.
What Are the Types of Medulloblastoma?
There are four main types of medulloblastoma that are primarily classified according to their molecular similarities. In the most recent WHO classification, these groups can be further subdivided. We will focus on the main four molecular categories here.
The four main types of medulloblastoma are listed below. In parenthesis is the approximate proportion of medulloblastoma cases that fall within this group:
- WNT-activated (10%): Usually occurs in children between the ages of 7 and 14, but also accounts for 15 - 20% of adult cases. Treatment is often effective. Good survival outcomes can be obtained in children, but less frequently for adults.
- SHH-activated (25%): This is the more common subgroup in adults and infants younger than 3 years of age. The prognosis of this subtype is highly variable, though in general lies between that of the WNT-activated and group 3 medulloblastomas.
- Group 3 (25%): This subtype is common in early childhood and is associated with a high rate of tumor spread (metastasis), frequently found at the time of diagnosis. Group 3 medulloblastomas are considered the most aggressive subtype and is associated with poor outcomes.
- Group 4 (40%): This is the most common type of medulloblastoma and affects males more often than females. Approximately a third of patients present with metastasis at diagnosis, and prognosis is generally intermediate.
What Are the Treatment Options?
Surgery, radiation therapy, and chemotherapy, often in combination, are used to treat medulloblastoma. Treatment regimens can differ based on age group. Initially, a special drain called an external ventricular drain (EVD) may need to be placed into the brain to remove excess CSF and relieve symptoms.
Surgery
Surgery is typically the first line of treatment for medulloblastoma. The goals of surgery are to remove as much tumor as is safely possible and to obtain tissue to confirm the diagnosis.
Performing total or near total resection of the tumor has a significant impact on survival and recurrence rates. Thus, having a competent and experienced neurosurgeon will be critical to maximize your chances of success.
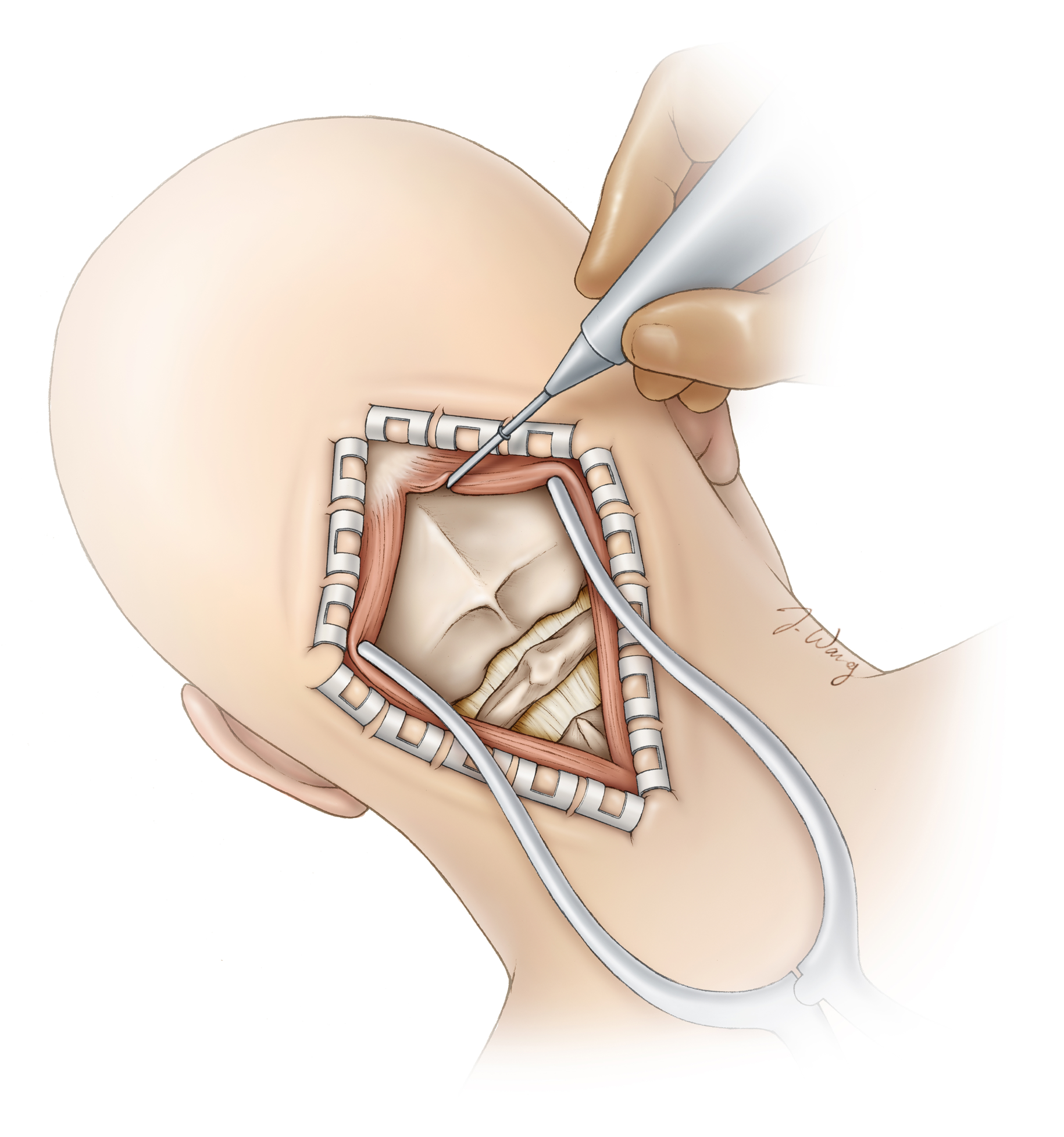
Figure 3: The scalp is retracted with special clips to prevent bleeding. Muscles are parted to reveal the skull bone. This bone will then be removed temporarily to access the brain.
Surgery will generally involve an incision in the scalp at the lower back part of the head and temporary removal of skull bone (craniotomy). After the skull bone is removed, the surgeon will use special surgical instruments to gently retract parts of the brain and remove the tumor.
Afterwards, the skull bone is replaced and secured back to the skull with metal plates. Patients may stay in the intensive care unit for a day or two before being transferred to the regular hospital ward. If an EVD was placed prior to surgery, it will be gradually removed after reducing the rate of drainage over time.
If the EVD cannot be removed (due to persistent blockage of CSF flow), a permanent shunt (ventriculoperitoneal shunt) may need to be placed.
Surgery to remove a medulloblastoma can be complex and may lead to various complications. Although surgeons do their best to minimize these risks, potential complications can include:
- Bleeding in the brain
- Infection at the site of surgery
- Swelling of the brain
- Leakage of CSF
- Damage to healthy brain tissue
- Cerebellar mutism syndrome, which can cause temporary loss of speech and emotional changes
Radiation
Radiation therapy involves the delivery of high-energy radiation beams to destroy cancer cells. For medulloblastoma, it is typically administered to the brain and along the entire length of the spine (craniospinal radiation), with a stronger dose targeting the tumor site. This is usually performed after surgery to inhibit growth from pieces of tumor left behind.
For infants and young children, radiation therapy is often avoided, reduced, or deferred due to the damaging effects of radiation on the growing brain. Complications of radiation therapy can include the following:
- Cognitive impairment, such as problems with memory, attention, and processing speed
- Hearing loss, which can be exacerbated by certain chemotherapy drugs like cisplatin
- Endocrine disorders, including growth hormone deficiency and thyroid problems, because radiation can affect the pituitary gland
- Secondary cancers caused by radiation exposure
- Radiation necrosis, where part of brain tissue is damaged
- Hair loss and skin irritation in the area being treated
Chemotherapy
Radiation therapy is usually followed by 4 to 9 cycles of chemotherapy. Typical agents include vincristine, cisplatin, carboplatin, or cyclophosphamide. These drugs are administered through a vein (intravenously).
Certain patients may also receive intrathecal chemotherapeutic agents, which involves delivering medications directly into CSF. This is often performed via a lumbar puncture (spinal tap), where a needle is inserted into the lower back to inject the chemotherapy drugs into the CSF.
Side effects of chemotherapy depends on the exact medication and dose, but can include nausea and vomiting, hair loss, fatigue, and decreased appetite. It can also increase the risk of infection. These effects are temporary and usually resolve after treatment.
What Is the Recovery Outlook?
The prognosis of a medulloblastoma diagnosis depends on a variety of factors such as its type, the amount of tumor removed during surgery, its response to treatment, and if it has metastasized.
In patients with non-metastatic disease who undergo successful surgery, radiation, and chemotherapy, the proportion of patients who are alive without recurrent disease at five years (5-year progression-free survival), is estimated as follows:
- WNT-activated: 95%
- SHH-activated: 70 - 80%
- Group 3: 50 - 60%
- Group 4: 70 - 80%
It is important to note that within these medulloblastoma types are several, more recently defined, subgroups. Each subgroup can exhibit differences in survival. Once a diagnosis is made, your medical team will discuss the outlook of your specific case with you.
Besides survival, understanding the projected quality of life will be important as you plan for what lies ahead. Despite relatively good survival outcomes for certain types of medulloblastoma, children have an increased risk of experiencing physical and mental disabilities that persist into adulthood.
This is because the treatments that address the tumor can also harm developing normal structures in the brain. Potential long-term effects may include reduced intelligence, processing speed, attention, memory, and executive function. Additionally, motor and behavioral changes can occur due to damage to the cerebellum.
In the last decade, significant progress has been made in understanding the biology of medulloblastoma. Researchers are looking to translate these findings into better treatment options. Enrolling in a clinical trial can offer access to new potential treatments. Discuss the availability, risks, and benefits of your options with your treatment team.
Key Takeaways
- Medulloblastoma is the most common malignant brain tumor of childhood.
- Symptoms can include nausea and vomiting, fatigue, and balance problems.
- Diagnosis is confirmed with imaging and a surgery/tissue biopsy to perform molecular tests.
- Surgery, radiation therapy, and chemotherapy are treatment options often performed in combination.
- Certain types of medulloblastoma have excellent survival outcomes, however, quality of life can be affected by the negative effects of treatment at an early age.











