Pituitary Tumor Resection: Surgery, Recovery, and What Patients Should Know
- What Is Pituitary Tumor Resection?
- When Is Pituitary Tumor Resection Needed?
- Types of Pituitary Surgery
- How Pituitary Tumor Resection Is Performed
- Benefits of Pituitary Tumor Resection
- Recovery After Pituitary Gland Resection
- Success Rates and Outcomes
- Choosing the Right Pituitary Surgeon
- Why Dr Aaron Cohen-Gadol Is a Trusted Pituitary Tumor Surgery Expert
- Conclusion
- Frequently Asked Questions
Resection is defined as surgically cutting out a tumor, tissue or part of an organ. Pituitary tumor resection is a highly specialized surgical procedure used to treat tumors and other disorders affecting the pituitary gland. Because the pituitary gland plays a central role in regulating hormones that control growth, metabolism, reproduction, and stress response, any condition that affects it can have widespread effects on the body. When medication or radiation therapy is not effective, pituitary tumor resection may be the most reliable way to relieve symptoms and restore hormonal balance.
Understanding how resection of a pituitary tumor works, when it is needed, and what recovery looks like can help patients and families feel more prepared and confident. This guide explains everything patients should know about pituitary gland resection, from diagnosis to long-term outcomes.
What Is Pituitary Tumor Resection?
The pituitary gland is a pea-sized organ located at the base of the brain, behind the nose, and below the optic nerves. Despite its small size, it is often called the master gland because it controls hormone production throughout the body. Resection of a pituitary tumor is performed by highly trained neurosurgeons, often working alongside endocrinologists and ENT (ear, nose, and throat) specialists.
Pituitary tumor resection is a surgical procedure most often performed to treat tumors on the pituitary gland. Rather than removing the entire gland, surgeons typically aim to excise only the tumor, preserving normal pituitary tissue whenever possible.
While it’s usually safe, the risks of this surgery include hormone changes, brain fluid leaks, and very rarely vision issues. Some cases require lifelong hormone replacement. Recovery time includes post-op care for nasal congestion and monitoring for potential hormonal imbalances.
When Is Pituitary Tumor Resection Needed?
Not all pituitary tumors require surgery. However, pituitary tumor resection may be recommended in several situations for different types of tumors.
- Hormone-secreting tumors that cause conditions such as Cushing's disease, acromegaly, or prolactin imbalance
- Macroadenomas (large tumors) that compress nearby structures, especially the optic nerves
- Vision loss or visual field defects caused by tumor growth
- Tumors unresponsive to medication
- Recurrent tumors after previous treatment
In these cases, pituitary tumor resection can relieve pressure on surrounding tissues, normalize hormone levels, and improve quality of life. The goal of resecting a pituitary tumor is to remove as much of the tumor as safely possible while minimizing risks.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Types of Pituitary Surgery
There are two primary surgical approaches used for pituitary gland resection, depending on the tumor’s size, location, and complexity.
1. Transsphenoidal Surgery
This is the most common approach for pituitary tumor resection. The surgeon accesses the pituitary gland through the nasal passages and sphenoid sinus, avoiding the need to open the skull. This minimally invasive method is often preferred because it leads to faster recovery, less pain, and fewer complications.
2. Craniotomy
In rare or complex cases, a craniotomy may be required. This procedure involves opening a portion of the skull to reach the pituitary gland. Although more invasive, this approach may be necessary if the tumor is very large or has spread into surrounding brain tissue. Even in these cases, the objective remains precise resection of pituitary tumor tissue.
How Pituitary Tumor Resection Is Performed
Before surgery, patients undergo detailed studies such as magnetic resonance imaging (MRI) scans and hormone evaluations. These tests help the surgical team plan the safest and most effective approach.
During surgery, advanced tools such as endoscopes, microscopes, and neuronavigation systems enable surgeons to access and visualize the tumor in great detail. In a typical pituitary tumor resection, done through the nose, ENT (ear, nose, and throat specialist) and neurosurgeons collaborate to carefully remove the tumor while protecting critical structures such as the optic nerves and normal pituitary tissue. Surgeons access the pea-sized gland at the base of the brain, behind the nasal passages, through the sphenoid sinus.
The procedure usually lasts several hours. After resection surgery, patients are monitored closely in the hospital to assess hormone levels, neurological function, and overall recovery.
Benefits of Pituitary Tumor Resection
The benefits of pituitary gland resection often outweigh the risks when surgery is recommended appropriately. Key benefits include the following:
- Relief from symptoms such as headaches, vision problems, and hormone imbalance
- Improved hormone regulation, which reduces the need for long-term medication
- Prevention of further tumor growth and therefore pressure on surrounding organs
- Improved quality of life and daily functioning
For hormone-producing tumors, pituitary tumor resection can be curative, especially when the entire tumor is removed. Even partial resection of a pituitary tumor can reduce symptoms significantly and improve treatment response.
Recovery After Pituitary Gland Resection
Recovery after pituitary tumor resection varies depending on the surgical approach used and individual patient factors. Most patients stay in the hospital for a few days after the surgery.
Short-Term Recovery
Patients may experience nasal congestion, fatigue, headaches, or mild discomfort. Hormone levels are closely monitored, and temporary or permanent hormone-replacement therapy might be needed after the resection of a pituitary tumor.
Long-Term Recovery
Full recovery can take several weeks. Patients are advised to avoid heavy lifting and strenuous activities during healing. Follow-up visits include imaging and blood tests to ensure that the tumor has not returned and hormone levels are stable.
Many patients report significant improvement in symptoms within weeks of pituitary tumor resection, especially when vision or hormone issues were present before surgery.
Success Rates and Outcomes
The success rate for pituitary tumor resection is generally high, especially when performed by an experienced surgeon at a specialized center. For small, well-defined tumors, complete pituitary tumor resection can achieve long-term control or cure.
Outcomes depend on several factors, including the following:
- Tumor size and type
- Whether the tumor secretes hormones
- The extent of resection of the pituitary tumor
- Patient’s overall health
Even when complete removal is not possible, partial pituitary gland resection often leads to symptom relief and improved effectiveness of additional treatments such as medication or radiation therapy.
Choosing the Right Pituitary Surgeon
Selecting the right surgeon is one of the most important decisions for patients considering pituitary gland resection. Key factors to consider include the following:
- Experience with pituitary tumor resection procedures
- Access to a multidisciplinary medical team
- Use of advanced surgical technology
- Clear communication and patient education
High-volume centers and surgeons who specialize in the resection of pituitary tumors tend to have better outcomes and lower complication rates.
Why Dr Aaron Cohen-Gadol Is a Trusted Pituitary Tumor Surgery Expert
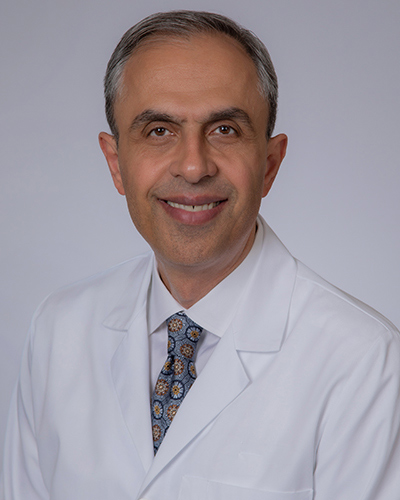
Dr Cohen-Gadol is widely recognized for his expertise in performing complex neurosurgical procedures, including pituitary tumor resections. With extensive experience in treating pituitary tumors, he is known for combining meticulous surgical technique with a patient-centered approach.
Dr Cohen-Gadol emphasizes preserving neurological and hormonal function while achieving maximal resection of pituitary tumor tissue. His use of advanced imaging, minimally invasive methods, and individualized treatment planning has made him a trusted choice for patients seeking expert pituitary surgery care.
Conclusion
Pituitary tumor resection is a highly effective treatment for many pituitary tumors and related disorders. When carefully planned and performed by an experienced specialist, pituitary tumor resection can relieve symptoms, restore hormone balance, and significantly improve quality of life. Understanding the surgical process, recovery expectations, and long-term outcomes empowers patients to make informed decisions.
If you or a loved one is facing pituitary tumor resection, choosing an experienced surgeon and a specialized medical center is essential. With modern techniques and expert care, pituitary tumor resection continues to offer excellent outcomes and renewed hope for patients worldwide.
Frequently Asked Questions
What happens if your pituitary gland is removed?
If the pituitary gland is partially or fully removed, you may need lifelong hormone-replacement therapy. However, with proper medical management, many people live healthy, active lives after pituitary gland removal.
What is the surgical removal of the pituitary gland?
The surgical removal of the pituitary tumor is called pituitary tumor resection, depending on whether only the tumor or part of the gland is removed.
Is pituitary gland surgery considered brain surgery?
Yes, pituitary gland resection is considered a form of brain surgery, even though many procedures are performed through the nasal passages rather than directly through the skull.