Spinal Cord Tumor: What the Patient Needs to Know
Overview
Spinal cord tumors are abnormal growths that develop within the spinal canal and compress the spinal cord. Patients may experience gradual sensory changes such as numbness or tingling, gait difficulty, weakness, loss of coordination, and pain of varying characteristics.
Treatment options include surgery, radiation, or observation in certain cases. Depending on the type of tumor and severity of symptoms before treatment, the recovery outlook for each patient varies. However, advances in surgical techniques and technologies have greatly improved patient survival and outcomes.
What Is a Spinal Cord Tumor?
Spinal cord tumors are abnormal growths that develop within the spinal canal. They can be classified as tumors that arise from within the spinal cord (intramedullary) or grow from cells surrounding the spinal cord (extramedullary). Extramedullary tumors can be further subdivided as tumors that are located inside or outside of the membranous covering of the spinal cord (dura).
Why should you have your surgery with Dr. Cohen?
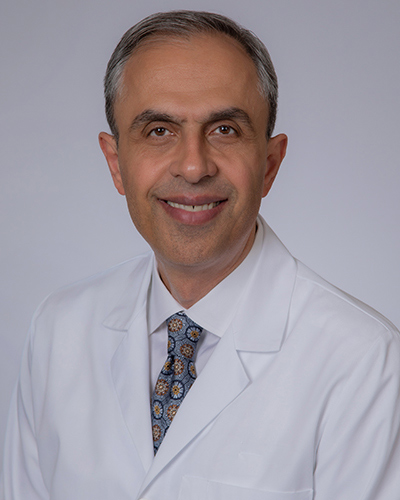
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.

Figure 1. Surgical removal of an intramedullary spinal cord tumor.
Intramedullary spinal cord tumors account for 8% to 10% of all primary spinal cord tumors. The majority of them are gliomas (ependymoma, astrocytoma) that originate from cells that surround and support neurons of the central nervous system. A small percentage of them are the hemangioblastoma subtype.
- Ependymoma (30%–40%)—well-circumscribed and slow-growing mass that typically affects adults in their third or fourth decade of life and is twice as common in men. Patients can present with sensory changes, loss of coordination, weakness, and pain.
- Astrocytoma (30%–35%)—ill-defined and infiltrative mass that typically affects adults in their third or fourth decade of life. Adults are more often seen with a tumor that can grow and spread more quickly (“high-grade”) than are children. Symptoms are like those caused by ependymomas. However, weakness is the predominant symptom in children.
- Hemangioblastoma (2%–15%)—small richly vascularized mass that typically affects adults in their third or fourth decade of life. Men are predominantly affected. Patients might experience symptoms similar to those caused by other spinal cord tumors, such as sensory disturbances (tingling or numbness), pain, and muscle weakness.

Figure 2. Surgical removal of an extramedullary spinal cord tumor (in orange).
Extramedullary spinal cord tumors account for 42% to 67% of all primary spinal cord tumors. Most (85%) of them are located within the dura and are considered intradural. The majority of them are meningiomas, nerve sheath tumors, or ependymomas.
- Meningioma (25%–46%)—well-circumscribed and slow-growing mass that typically affects elderly patients in their seventh decade of life (75%) and young adults aged 25 to 35 years. Females are more commonly affected. The most commonly reported symptoms include back pain, sensory changes, weakness, and problems with walking.
- Nerve sheath tumors (34%)—this group of tumors includes schwannomas (92%), neurofibromas, and malignant peripheral nerve sheath tumors. Schwannomas are usually sporadic, whereas neurofibromas are encountered in patients with neurofibromatosis type 1. Pain is the predominant symptom, but weakness, tingling sensations, problems with walking, and bladder dysfunction have been reported.
- Ependymoma (6%–7%)—rare and slow-growing tumor that occurs in the lower back regions of the spinal canal. Such tumors arise from the ependymal cells lining the spinal canal and typically affect patients in their fourth decade of life. Back pain is the major symptom. This is often accompanied with weakness, sensory disturbances, and bladder dysfunction.
What Are the Symptoms?
Most patients present with slow and progressive sensory changes (tingling or numbness), loss of coordination, gait difficulty, weakness, and pain of various quality depending on the location and type of the tumor involved.
What Are the Causes?
The cause of spinal cord tumors is not currently known. Certain inherited disorders such as neurofibromatosis 1, neurofibromatosis 2, and von Hippel-Lindau disease are prone to cause the development of benign central nervous system tumors.
How Common Is It?
Spinal cord tumors are rare and account for 2% to 4% of all central nervous system tumors. Some are more common in males (for example, hemangioblastoma), whereas others are more common in females (for example, meningioma). Most subtypes affect adults in their third or fourth decade of life.
How Is It Diagnosed?
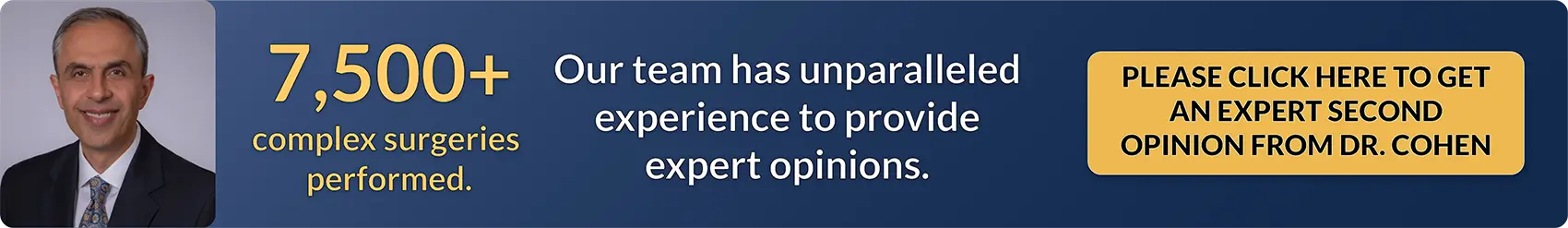
Spinal cord tumors are usually diagnosed by magnetic resonance imaging (MRI). MRI can help define the interface between the tumor and spinal cord and identify associated cysts and bleeding. Spinal X-ray images might be obtained to investigate the bony anatomy, the alignment of the spine, and spinal stability.
Figure 3. Spinal cord tumor with minimal enhancement (left) associated with a small bleed (red arrow, right).
What Are the Treatment Options?
Spinal cord tumors are treated primarily with surgery and radiotherapy. If the tumor is found incidentally and does not cause symptoms, the best course of treatment varies depending on the nature of the tumor involved and the patient’s age, health, and preference.
Observation
Patients who have no symptoms but are diagnosed incidentally can be observed over time. Slow-growing tumors such as meningiomas and schwannomas can be followed with regular imaging, especially in older patients. However, the best approach must be tailored to each patient.
Surgery
Surgery is usually indicated if the tumor causes symptoms. The goal is to remove as much tumor as possible without damaging the spinal cord. Tumors that have spread widely into nearby spinal cord tissue are typically not cured by surgery. However, surgery is often performed initially to reduce the amount of tumor (relieve the tumor pressure on the spinal cord) for later radiation or chemotherapy. After surgery, the patient is observed in the intensive care unit overnight. Depending on the complexity of the surgery, patients might stay in the hospital for a few days or longer.
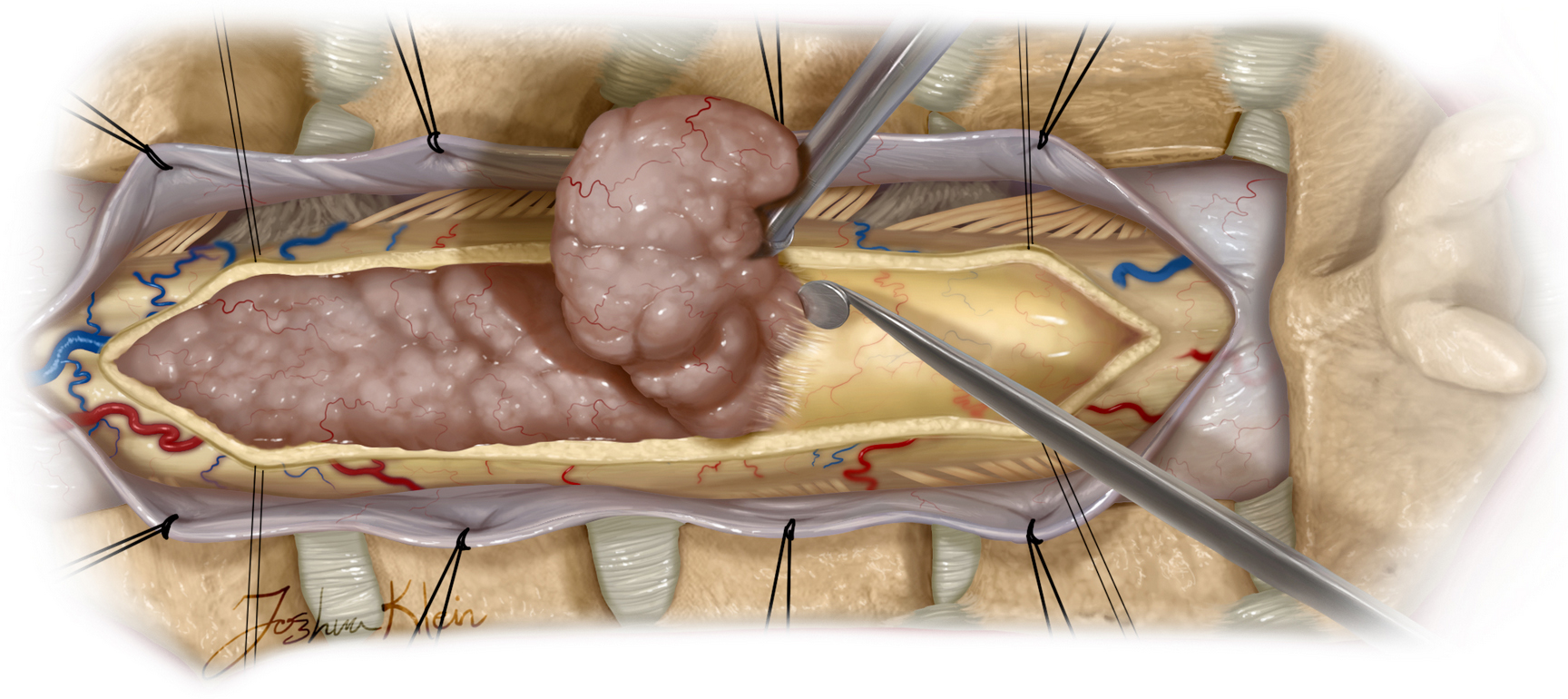
Figure 4. The spinal cord is opened, and the tumor is carefully peeled off.
The surgical approach involves placing the patient on his or her stomach and making a cut along the line of the spine where the tumor is located. The surgeon removes the top parts of the bony spine, opens the layers covering the spinal cord, makes a cut parallel to the spinal cord fibers (if needed), and gently removes the tumor.
Depending on the type of tumor, the number of blood vessels involved, and the extent to which the tumor has spread to nearby tissues, tumor removal during surgery can be associated with complications, including worsening sensory and motor symptoms, cerebrospinal fluid leak, and infection.
In this video, Dr. Cohen describes the techniques for surgery to treat a large cervical spinal cord ependymoma.
For more information about the technical aspects of the surgery and extensive experience of Dr. Cohen, please refer to the chapter on Intramedullary Spinal Cord Tumor in the Neurosurgical Atlas.
Radiation
Radiation is another option for treating spinal cord tumors and can be used in combination with surgery when the tumor cannot be removed completely. There are multiple ways to delivery this treatment; radiosurgery, fractionated radiotherapy, and brachytherapy are among the more common options.
During radiosurgery, hundreds of small, concentrated beams of radiation are aimed at the tumor using a radiosurgical device. The procedure takes 30 to 50 minutes,
The patients who undergo fractionated radiotherapy receive smaller doses of radiation over several visits. Each visit takes only 5 to 15 minutes, and the patient is able to go about his or her business before and after the visit.
Brachytherapy delivers radiation by directly applying a radiation source near the tumor, which can be done during surgery or after the surgery through the skin. This option is usually considered after other options have been exhausted.
It is important to note that radiation therapy does not remove the tumor. It can, in some cases, cause the tumor to shrink. The main goal of radiation is to stop the tumor from growing. As a result, the patient must return for MRI scans on a yearly basis to check for any new growth.
Possible complications of radiation therapy depend on which part of the spine is treated and include skin redness at the site of radiation application and sore throat. Radiation-induced spinal cord injury is another possible complication of radiotherapy that results in weakness, sensory changes, clumsiness, and/or pain. This complication is very rare but can occur months to years after treatment.
What Is the Recovery Outlook?
The outcome for patients with a spinal cord tumor depends on the type of tumor, how involved the tumor is with the spinal cord, the extent of spread to nearby tissues, and the severity of symptoms before treatment. Advances in surgical techniques and technologies have improved the safety and efficacy of spinal cord tumor therapies. Patients should discuss what to expect after treatment with their physician.
Resources
Glossary
Cerebrospinal fluid—clear fluid surrounding the brain and spinal cord
Dura—outermost layer of the meninges
Meninges—outer membranous covering of the brain and spinal cord
Contributor: Gina Watanabe BS
References
- Chamberlain MC, Tredway TL. Adult primary intradural spinal cord tumors: a review. Curr Neurol Neurosci Rep 2011;11:320–328. doi.org/10.1007/s11910-011-0190-2
- Samartzis D, Gillis CC, Shih P, O’Toole JE, Fessler RG. Intramedullary spinal cord tumors: part I—epidemiology, pathophysiology, and diagnosis. Global Spine J 2015;5:425–435. doi.org/10.1055/s-0035-1549029
- Sandalcioglu IE, Gasser T, Asgari S, et al. Functional outcome after surgical treatment of intramedullary spinal cord tumors: experience with 78 patients. Spinal Cord 2005;43:34–41. doi.org/10.1038/sj.sc.3101668
- Tobin MK, Geraghty JR, Engelhard HH, et al. Intramedullary spinal cord tumors: a review of current and future treatment strategies. Neurosurg Focus 2015;39:E14. doi.org/10.3171/2015.5.FOCUS15158