Arteriovenous Fistula: What the Patient Needs to Know

Overview
An arteriovenous fistula (AVF) is an abnormal connection between an artery and a vein. Intracranial AVFs often refer to those that form near the outer covering of the brain (dura) and are called dural AVFs (dAVFs). Symptoms depend on the location of the fistula and can include headaches, pulsating ringing of the ears (tinnitus), and vision changes. Treatment options include observation, endovascular embolization, surgery, or radiosurgery or a combination of these treatments.
What Is an Arteriovenous Fistula?
An AVF is an abnormal connection between an artery and a vein. Normally, blood flows from arteries to capillaries and then to veins. Capillaries are thin blood vessels that allow for the transport of nutrients and oxygen into tissues. In a fistula, blood flows directly from high-pressure arteries to low-pressure veins, bypassing the capillary network. Tissues near these capillaries may suffer damage from the lack of blood.
AVFs can occur anywhere in the body. They can even be surgically made for dialysis in patients with severe kidney disease. When a fistula occurs within brain tissue, it is called an arteriovenous malformation. When a fistula occurs near the outer covering of the brain (dura), it is called a dAVF.
Some fistulas between specific arteries and veins have their own names. For example, a carotid cavernous fistula (CCF) shunts blood from the carotid artery to the cavernous veins. Symptoms of an AVF are variable and depend on its location and the amount of blood being shunted.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.

Figure 1. The location and incidence of the most common types of intracranial dAVFs. Depicted in blue are the brain’s venous sinuses, which drain blood back to the heart.
What Are the Symptoms?
dAVFs near the transverse-sigmoid sinus (Figure 1) typically present with a pulsating ringing in the ears (tinnitus). Other symptoms might occur due to the high blood pressure in the veins, bleeding, or lack of oxygen delivered to tissues near the fistula. These symptoms include headaches, nausea, vomiting, seizures, speech or language problems, dementia, unsteadiness, vision deterioration, and bulging of the eyes.
What Are the Causes?
dAVFs do not have a well-defined cause. Surgery, head trauma, and hereditary vascular or coagulation diseases (antithrombin, protein C deficiency, protein S deficiency) can increase the risk of AVF formation.
How Common Is It?
dAVFs are rare and account for 10% to 15% of arteriovenous malformation cases. The frequency of arteriovenous malformations in the general population is approximately 0.15%. Symptoms usually present between 50 and 60 years of age.
How Is It Diagnosed?
dAVFs are diagnosed by computed tomography (CT) or magnetic resonance imaging (MRI) and angiography. Imaging might show dilated blood vessels with congestion of blood in the veins and signs of high blood pressure or bleeding. Abnormal blood flow around the large veins near the dura prompts closer investigation with angiography.
Angiography is a minimally invasive procedure that involves placing a catheter into an artery, passing it through blood vessels to the brain, and then injecting a contrast dye near the blood vessels of interest. X-ray images and videos are then taken to visualize the structure of the blood vessels and blood flow from the arteries to veins.
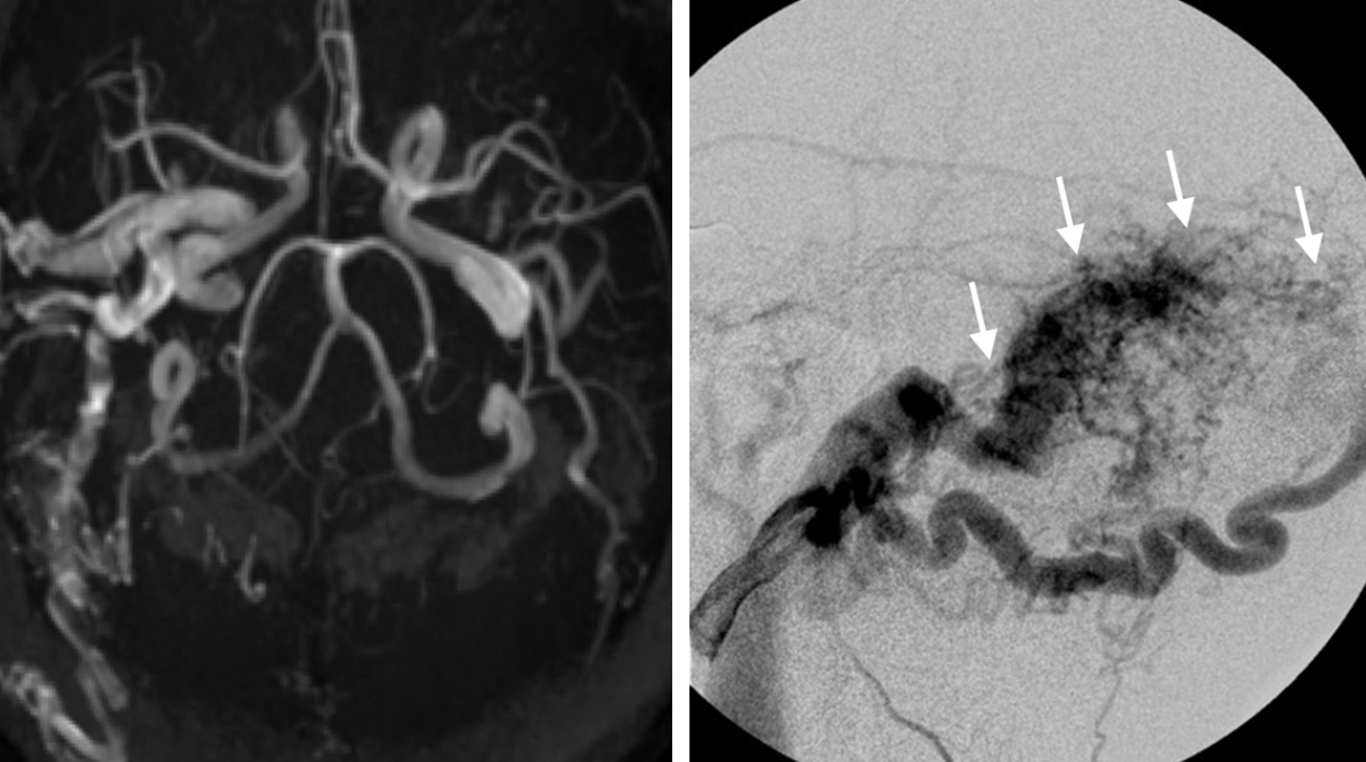
Figure 2. Angiograms showing abnormal blood flow (left) and a transverse-sigmoid sinus dAVF (right, white arrows).
What Are the Treatment Options?
dAVF treatment options include observation, embolization, and surgery. The risk of treatment should be weighed against the expected clinical course of the fistula. Fistulas that drain into veins that run along the grooves/surface of the brain (cortical veins) should be treated early to avoid the risks of bleeding and neurologic problems. Other fistulas, especially if they do not cause symptoms, can be observed over time.
Observation
Patients with a fistula that has a lower risk of bleeding can be observed over time. Angiography might be performed every 3 to 5 years to check for any change in the pattern of blood flow.
Embolization
Embolization is the primary mode of treatment for dAVFs. Embolization uses the same initial procedure as diagnostic angiography, in which a catheter is passed through an artery at the top of the leg and then guided to the blood vessels of the dAVF. Instead of injecting a contrast dye, an occluding material such as a special glue is delivered to the blood vessels of the dAVF to block off abnormal blood flow.
The procedure can take 3 to 8 hours and is followed by at least an overnight hospital stay. The length of stay is variable; the patient might stay in the hospital for several days while being observed. A single procedure is often all that is needed to eliminate the dAVF.
Possible complications of embolization include stroke and rebleeding (if the fistula is not completely blocked off) and neurologic problems (due to changes in blood flow). Other complications are specific to the occluding agent used and can include cranial nerve injury and blood vessel toxicity. Embolization might be used in combination with surgery.
Surgery
For cases in which endovascular embolization has failed or is not possible, surgical resection might be performed. The surgeon disconnects the involved arteries and veins and cuts away abnormal dura. Before the operation, embolization might be used on the arteries of the fistula to reduce blood loss. During the operation, angiography might be used to identify the involved blood vessels and ensure complete obliteration of the fistula.
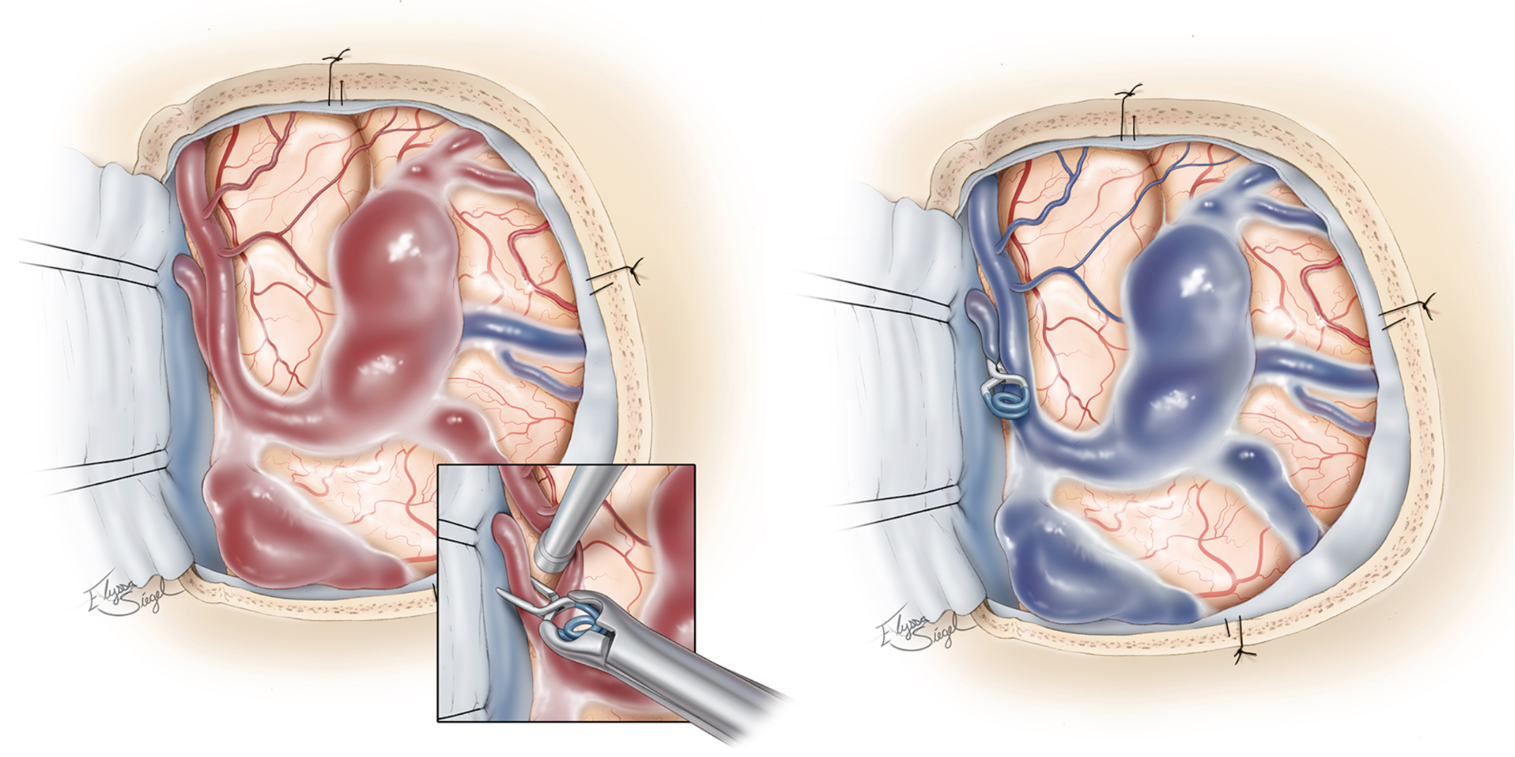
Figure 3. Clipping of a vein of a fistula at the site of its abnormal connection to an artery (left) and resulting occlusion of the fistula and return of normal venous blood flow (in blue) (right).
Complications of surgery include infection, excess fluid within the cavities of the brain (hydrocephalus), cerebrospinal fluid leak, stroke, severe blood loss, and loss of function in cranial nerves.
In this video, Dr. Cohen describes the techniques for surgery to treat a dural arteriovenous fistula.
For more information about the technical aspects of the surgery and extensive experience of Dr. Cohen, please refer to the chapter on Principles of Dural Arteriovenous Fistula Surgery in the Neurosurgical Atlas.
Radiosurgery
Radiosurgery aims hundreds of low-dose beams of radiation at the abnormal vessels of the dAVF using technologies such as the Gamma Knife or Novalis. The goal is to injure the cells of the abnormal connecting vessels periodically until scar tissue forms, which can close off blood supply to the dAVF and eventually close off the fistula. The procedure is painless; it can take several hours of preparation and 1 hour for the delivery of radiation. The patient can go home the same day.
This is usually the last treatment option considered because obliteration of the dAVF can take months to years and might not completely close off the fistula. During this time, there is still a risk of bleeding. Experience with radiosurgery for the treatment of dAVF is growing. This approach should be reserved for carefully selected cases that have exhausted other treatment options.
Complications of radiosurgery include nausea, vomiting, seizures, and headaches. Several complications, such as hemorrhage, death of healthy tissue around the site of radiation (radiation necrosis), and brain swelling (edema) can occur weeks to years after treatment.
What Is the Recovery Outlook?
Complete cure involves occluding the fistula by closing the fistula through embolization or surgery. A combination of the treatments discussed above might be necessary. After surgery, it can take 4 to 6 weeks to go back to performing usual activities; full recovery requires up to 2 to 6 months. However, the speed of recovery for each person varies. If the surgery affected your speech or ability to perform daily activities, your doctor might recommend working with a speech or occupational therapist.
Resources
Glossary
Dural venous sinus—channels of deoxygenated blood drained from the cranial cavity and routed back to the heart
Edema—swelling of the brain
Radionecrosis or radiation necrosis—death of healthy tissue surrounding the site of radiation
Hemorrhage—bleeding from a blood vessel
Catheter—thin, hollow, flexible tube
Stroke—condition that occurs when blood supply to a part of the brain is interrupted or reduced, which prevents the delivery of oxygen and nutrients to brain tissues
Embolization—blockage of a blood vessel so that blood cannot flow through it
Contributor: Gina Watanabe BS
References
- Gandhi D, Chen J, Pearl M, et al. Intracranial dural arteriovenous fistulas: classification, imaging findings, and treatment. Am J Neuroradiol 2012;33:1007–1013. doi.org/10.3174/ajnr.A2798
- Baharvahdat H, Ooi YC, Kim WJ, et al. Updates in the management of cranial dural arteriovenous fistula. Stroke Vasc Neurol 2020;5. doi.org/10.1136/svn-2019-000269











