What You Should Know About Cavernous Malformation Surgery


Cavernous malformations or cavernomas, are clusters of enlarged and deformed blood vessels. They can occur anywhere in the body but are more concerning when found in the brain or spinal cord. When symptoms are present or the risk of hemorrhage and future neurological impairment is high, treatment may be needed.
Fortunately, surgery can completely remove a cavernous malformation and provide a cure for this condition. It will be important to weigh the risks and benefits of surgery before pursuing this treatment option.
If you decide to proceed with surgery, the months and days leading up to the date of the operation can be terrifying. Knowing what exactly the surgery will entail can help to alleviate some of the concerns and anxiety. In this article, we discuss the risks and benefits of surgery, along with the general steps of the surgical procedure.
What Is a Cavernous Malformation?
A cavernous malformation is a group of abnormally formed blood vessels composed of irregular thick and thin walls. Cavernomas can range widely in size but are typically 1 to 5 cm (about 0.5 to 2 inches) in diameter.
Cavernous malformations go by many other names: cavernous hemangioma, cavernoma, cavernous angioma, angioma, and hemangioma are all terms that are used to refer to a cavernous malformation.
Cavernous malformations located in the brain can also be called cerebral cavernous malformation. To keep things simple, we will use “cavernous malformation” throughout the article and focus on only cavernous malformations that occur in the brain.
Treatment for Cavernous Malformations
Cavernous malformation treatment guidelines were proposed by the Angioma Alliance scientific advisory board clinical experts panel in 2017.
The treatment guidelines consider the presence of symptoms, the risk of future bleeding, the location of the cavernous malformation, and patient preference when deciding whether surgery is beneficial.
In general, if the cavernous malformation causes problematic symptoms such as seizures and resides in an easily surgically accessible location, cerebral cavernous malformation surgery may be a good option.
In contrast, if the cavernous malformation produces no symptoms or is in a deep or surgically inaccessible location, surgery will be less beneficial and more risky. Observation may be more appropriate.
Each patient will have a unique situation. A thorough discussion of the risks and benefits of surgery with your neurosurgeon will be important to determine if cavernoma surgery or another treatment option will be right for you.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Cavernous Malformation Surgery Success Rate and Risks
Following surgery, more than 80% of patients experience improvement in symptoms and are satisfied with the procedure. Many patients may no longer have seizures, although this may be less likely for patients who experienced seizures over longer periods.
Up to 60% of patients with cavernous malformations located near a critical area of the brain such as the brainstem will also have symptom improvement after surgery.
When surgery is performed by a skilled and experienced neurosurgeon, death resulting from surgery is extremely unlikely.
Even in cases of cavernous malformations located in the brainstem, mortality is reported in less than 1% to 2% of cases. Immediately after the operation, approximately 5% of patients may experience new worsening of symptoms, but most patients will recover over time.
The success of surgery highly depends on the expertise of the neurosurgeon. Deciding on a neurosurgeon for your care will be a critical aspect in the treatment process.
Learn more about how to find the top expert for your surgery, and when and how to seek a second opinion in our other articles.
What Does Cavernous Malformation Surgery Entail?
Cavernous malformation surgery can last 4 to 6 hours or longer depending on the complexity of your case. Here we describe the general steps taken to remove a brain cavernous malformation.
Step 1: Patient Positioning
The patient is placed on the operating table and is given general anesthesia. Once asleep, a breathing tube is placed in the windpipe (trachea) and connected to a ventilator to pump oxygen to the lungs during the operation.
A 3-pin clamp is connected to the operating table and attached to the patient’s head for immobilization. Hair is shaved near the incision site.
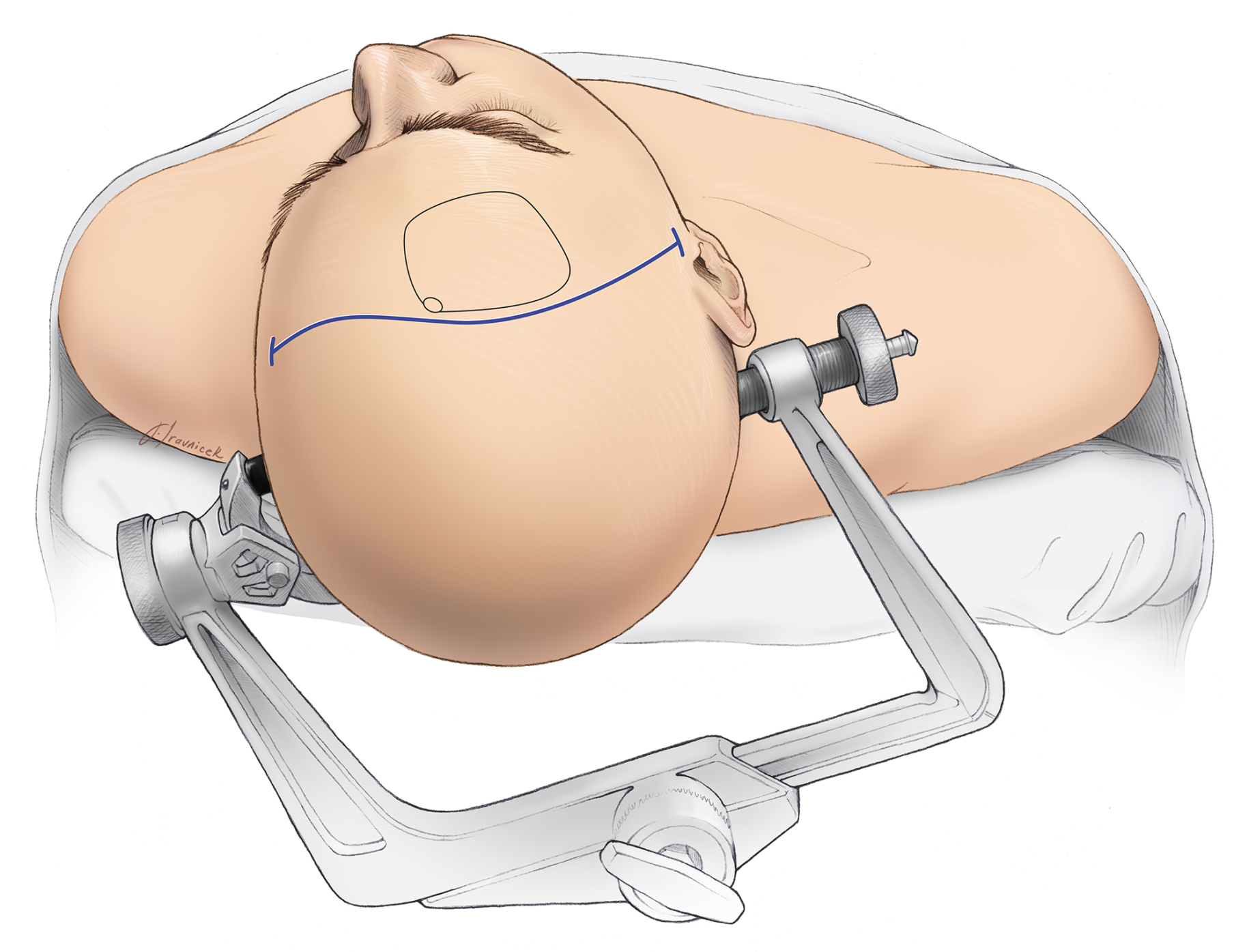
Figure 1: A 3-pin skull clamp is used to fix the head in the optimal position for surgery.
Step 2: Skin Incision
The skin is scrubbed with antiseptic before an incision is made through the scalp to the outer surface of the bone. Clips are applied to the edges to minimize bleeding.

Figure 2: The scalp is cut and clips are applied to minimize bleeding. A blunt tool can be placed over the muscles to prevent damaging any blood vessels.
Step 3: Craniotomy
If any muscles are present, they are flapped back and secured. A small opening in the skull is made using a surgical drill (burr hole). A blunt tool is inserted into the burr hole and used to gently separate the bone from the outer covering of the brain (dura).
A saw-like instrument called a craniotome is then used to cut the bone and create a removable bone flap.
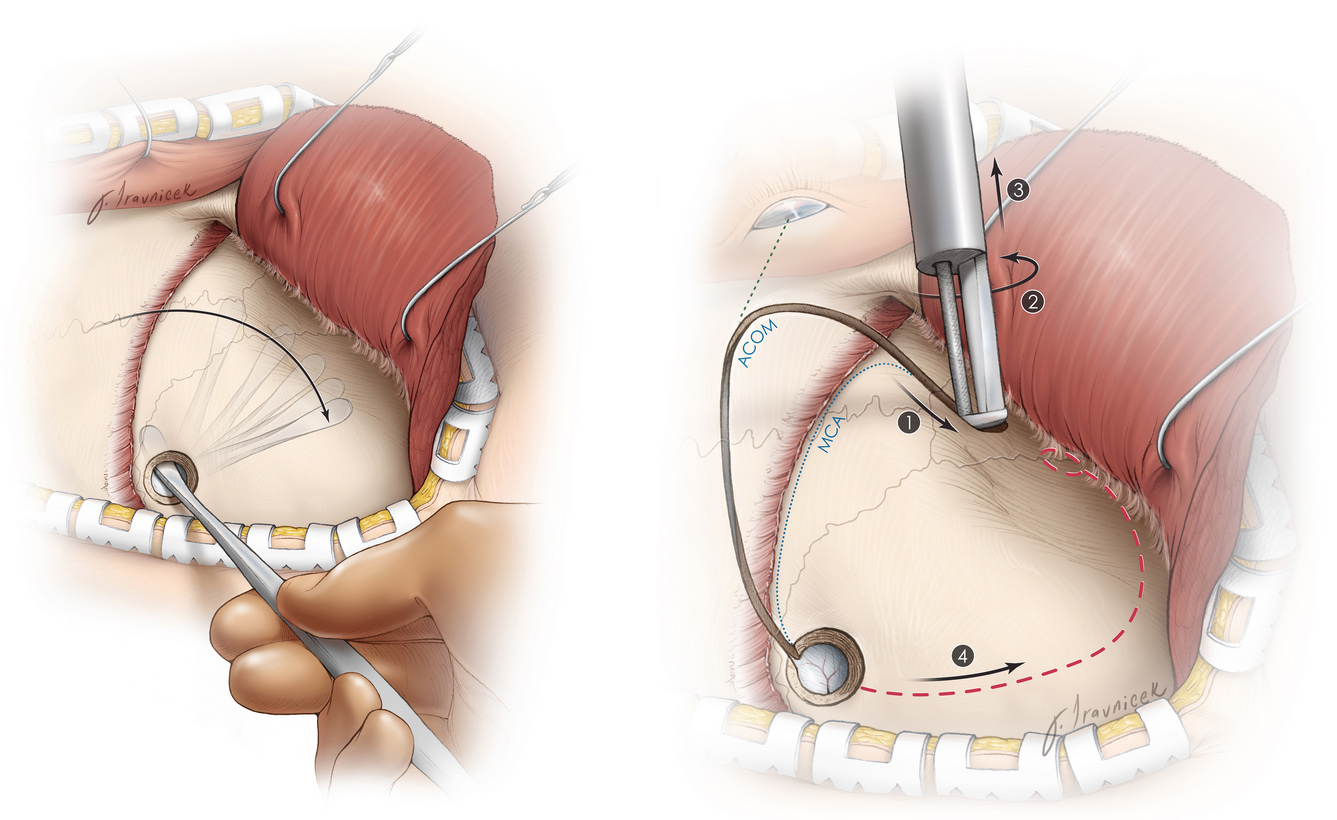
Figure 3: A blunt dissector separates the inner bone from the membranous covering of the brain (left). Afterward, the craniotome saws through the bone (right).
Step 4: Brain Exposure and Cavernous Malformation Removal
The dura is carefully cut with small scissors and flapped back, allowing the brain to be exposed. Surgical instruments are used to find and reach the cavernous malformation.
Once identified, the cavernous malformation is disconnected from the surrounding brain tissue. Following removal, the cavity is inspected for any bleeding or remnants.

Figure 4: Complete removal of a cavernous malformation around its capsule.
Cavernous Malformation Surgery Recovery
After cavernous malformation surgery, the recovery journey begins. The timeline for cavernous malformation recovery varies for each patient.
Complete recovery may take 4 to 6 weeks or longer depending on the complexity of the case and any underlying medical conditions.
Immediately after surgery, you may need to stay in the intensive care unit overnight for monitoring and management of any swelling, bleeding, or neurological problems before being transferred to a regular hospital room. If there are no complications, most patients can go home within 3 to 5 days.
Post-Operative Care
On average, recovery can take around six weeks. The recovery period will depend on factors such as your overall health and age. Strenuous activity and tasks like driving should be restricted, so it’s highly recommended that patients seek assistance from family, friends, or professional caregivers to manage their errands and household tasks during this period.
Side effects such as fatigue, headaches, and bouts of nausea are common. During this time, your doctor will schedule follow-up appointments to monitor your recovery and can prescribe medications to manage the symptoms. They will advise you when you can gradually resume regular activities.
If your cavernoma surgery is successful, your condition should improve and its symptoms should be completely resolved. However, there are also risks associated with surgery, which could lead to complications, such as:
- Stroke
- Temporary or permanent neurological impairments
- Swelling or bleeding in the brain
Seek immediate medical attention if you notice any of these complications. Your surgeon may recommend periodic MRI or CT scans to ensure there are no underlying complications or adjust your recovery plan as needed.
How Serious is Cavernoma Surgery?
Cavernoma surgery is considered a serious procedure because it involves operating on delicate areas of the brain or spinal cord, where even small changes can impact important functions. The goal of surgery is to safely remove the cavernous malformation to prevent seizures, future bleeding, or neurological deficits, but the risks depend on the location and size of the lesion. Cavernomas situated in deep or highly sensitive areas of the brain may pose greater surgical challenges, increasing the potential for complications such as weakness, vision changes, speech difficulties, or coordination problems.
However, in experienced neurosurgical centers, many patients undergo cavernoma surgery successfully with significant improvement in symptoms and reduced risk of future hemorrhage. The seriousness of the procedure highlights the importance of thorough evaluation, advanced imaging, and careful surgical planning. While cavernoma surgery carries risks, it can be life-changing or even lifesaving for patients experiencing recurrent bleeds or disabling symptoms.
Key Takeaways
When performed by a skilled and experienced neurosurgeon, cavernous malformation surgery is safe and can provide symptom relief. However, the likelihood of benefit and the risk of surgery varies for each patient. It will be important to have a thorough discussion of the potential risks and benefits of surgery with your neurosurgeon.











