Chordoma: What the Patient Needs to Know

What Is a Chordoma?
A chordoma is a rare type of tumor that occurs in the spine or base of the skull. Chordomas arise from the remaining pieces of the notochord, a rodlike structure important during embryonic spine development but broken down by the time we are born. Although chordomas are not particularly known to spread to other parts of the body (metastasize), the tumor may eventually grow and invade surrounding structures, including bone. Approximately half of all chordomas occur at the spine, with the tailbone and the base of the skull serving as other common locations.
What Are the Symptoms?
The symptoms of a chordoma tumor vary and depend on its location and size. Chordomas can arise anywhere along the spine, from the skull base to the tailbone.
A skull base chordoma may present with vision problems (for example, double vision), headaches, vertigo, hearing loss, numbness, difficulty swallowing, or facial pain.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
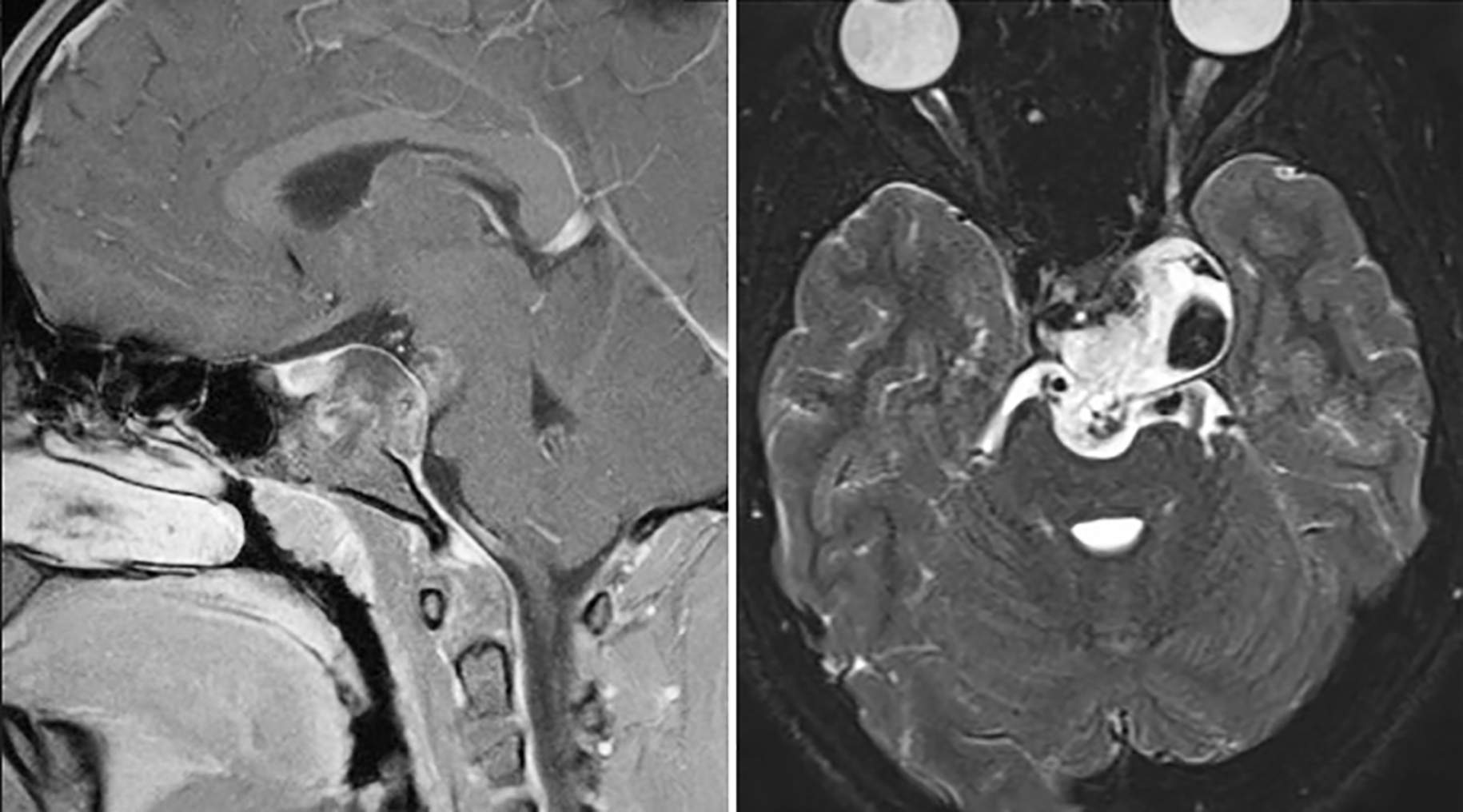
Figure 1. A chordoma is shown centered and pushing against normal brain on magnetic resonance imaging (MRI) from side (left) and top-down (right) views.
A chordoma at the lower spine presents differently than one at the skull base. Common symptoms include lower back pain or numbness, changes in bowel habits, incontinence, impotence (in men), and changes in mobility. Symptom onset can be gradual or relatively rapid if the tumor is aggressive.
What Are the Causes?
The underlying cause of chordomas is currently unknown. However, researchers have linked chordomas to abnormalities of the T gene on chromosome 6. This gene encodes a protein important in notochord development.
How Common Is It?
Chordomas are rare, with approximately 1 case diagnosed per million people. Overall, males are more commonly affected than females in an approximately 2:1 ratio. Most patients harboring a chordoma are between 40 and 70 years of age at the time of diagnosis.
How Is It Diagnosed?
Chordomas are diagnosed with the help of computed tomography (CT) and magnetic resonance imaging (MRI) scans, which examine the bone and soft tissue in detail. A contrast dye might be used to highlight the tumor.
To confirm the diagnosis, a section of tumor is removed for microscopic examination by a pathologist (biopsy). The biopsy allows for specific diagnosis and can measure how aggressively the tumor is growing (its malignancy).
Depending on what other structures are affected by the tumor, the physician might choose to order a variety of other laboratory or neurologic tests to evaluate the patient’s overall health and neurologic function.
What Are the Treatment Options?
The course of treatment for a chordoma depends on the tumor’s size, location, and degree of spread, as well as the patient’s age and overall health. Treatments include surgery, radiation therapy, chemotherapy, or a combination of these treatments.
Surgery
Surgery to remove as much of the tumor as possible is the preferred primary treatment. The percentage of tumor that can be removed will depend highly on the size and location of the growth.
It might not be possible to totally excise tumors adjacent to or encapsulating certain nerves, blood vessels, or important parts of the brain/spinal cord.
For tumors located at the base of the skull, the surgeon might use a procedure known as the expanded endonasal transsphenoidal approach to access and remove the tumor through the nose (Figure 2).
Endoscopic methods (which involve using small cameras to see around corners and maximize tumor removal) might be used. Other methods of surgical resection will depend on the tumor’s overall size, shape, and location.
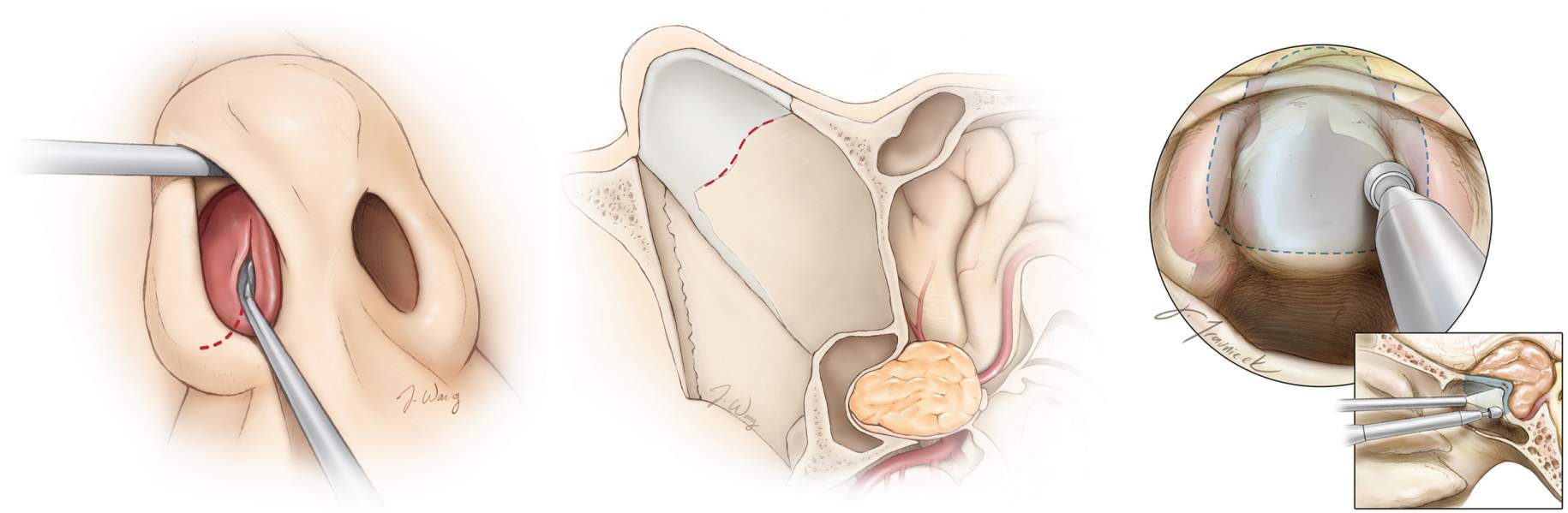
Figure 2. The expanded endonasal transsphenoidal approach allows the surgeon to access the tumor through the nose in a minimally invasive fashion.
The surgery takes approximately 2 to 6 hours depending on the location and size of the tumor. After surgery, you will be observed in the intensive care unit overnight and then transferred to a private room the next day.
There will be some discomfort in and around the nose, but this is usually not very bothersome. You may be discharged from the hospital within a few days.
During surgery, if the tumor is invading or attached to the membranes around the brain (dura), attempting to remove the tumor might tear these membranes and cause leakage of brain fluid (cerebrospinal fluid) from the nose after surgery.
If this is the case, your hospitalization may be prolonged by a few days to allow the surgeon to fix the leakage by placing a small tube in your back (lumbar drain) or a short second surgery to repair the leakage site. If the leakage is not corrected, the chance of infection (meningitis) increases.
Depending on the extent of your surgery, you may return to your daily activities shortly after discharge from the hospital. Any leakage of clear fluid from your nose should be reported to your surgeon.
Radiation Therapy
Radiation therapy often follows surgical removal but also might be used in instances of tumor recurrence or an inoperable tumor. Radiation therapy is more often used to treat chordomas than chondrosarcomas.
There are several ways to administer radiation therapy. External-beam radiation involves high-energy radiation applied to the site of interest. Treatment usually occurs 5 times a week over the course of several weeks.
Stereotactic radiosurgery can apply higher doses of radiation to a smaller area. The radiation dose may be broken up over multiple beams.
Using the radiological imaging data, your surgeon and radiation oncologist can deliver the radiation more precisely while avoiding healthy tissues. It is an outpatient procedure and is usually done in 1 session.
All forms of radiation therapy carry some risk of damage to normal tissues. Specifics should be discussed with your radiation oncologist and surgeon.
Chemotherapy
Chemotherapeutic agents target the rapidly dividing cells of tumors and are rarely used to treat chordomas. These drugs also damage normal cells in the body that may frequently divide, resulting in adverse effects such as hair loss and anemia. The doctor may prescribe other medicines used to control or manage the symptoms associated with these tumors.
Chordoma Prognosis: What Is the Recovery Outlook?
Although tumor growth tends to be slow, the rate of recurrence for these tumors is high, and frequent follow-up observation is necessary to monitor for such recurrences. Keep a strict schedule of follow-up appointments, scans, and any additional tests.
The median survival rate is estimated to be 6 to 7 years. Patients should seek care from specialized oncologists and neurosurgeons with expertise in treating this rare type of tumor.
Coping With Chordoma
It’s normal to experience a range of emotions after being diagnosed with chordoma. Professional support from counselors and joining support groups can significantly affect your emotional well-being.
When it comes to managing symptoms, chordoma patients may experience minimal or no symptoms at first. However, the tumor can press on nerves and vital structures as it grows, leading to symptoms such as headaches, double vision, neck pain, or issues with bowel and bladder function, depending on its location. Early recognition of symptoms and seeking a surgical evaluation is crucial for effective treatment.
You may also need to adapt your lifestyle to fit your capabilities. This could involve modifying your home, adjusting your work life, and adopting a balanced diet and gentle exercise routine to help manage symptoms and improve overall health.
Depending on the progression of the disease, chordoma can also lead to varying levels of disability. Accessing rehabilitation services and utilizing assistive devices can help you maintain independence and improve quality of life.
Living with chordoma involves understanding your condition, connecting with the right healthcare providers, and prioritizing your physical and mental health. By staying informed, actively participating in your treatment decisions, and seeking support from the chordoma community, you can navigate this journey with strength and resilience.
Resources
Glossary
Cerebrospinal fluid—clear fluid surrounding the brain and spinal cord
Biopsy—test to examine tissue removed from a living body
Dura—outermost membrane covering the brain and spinal cord
Meningitis—inflammation/infection of the membranes covering the brain and spinal cord
Malignancy—tendency to become progressively worse
Metastasize—spread of a cancer to other sites in the body
Contributor: Gina Watanabe BS
References
- Jones PS, Aghi MK, Muzikansky A, et al. Outcomes and patterns of care in adult skull base chordomas from the Surveillance, Epidemiology, and End Results (SEER) database. J Clin Neurosci 2014;21:1490–1496. doi.org/10.1016/j.jocn.2014.02.008
- Walcott BP, Nahed BV, Mohyeldin A, et al. Chordoma: current concepts, management, and future directions. Lancet Oncol 2012;13:e69–e76. doi.org/10.1016/S1470-2045(11)70337-0











