Oligodendroglioma

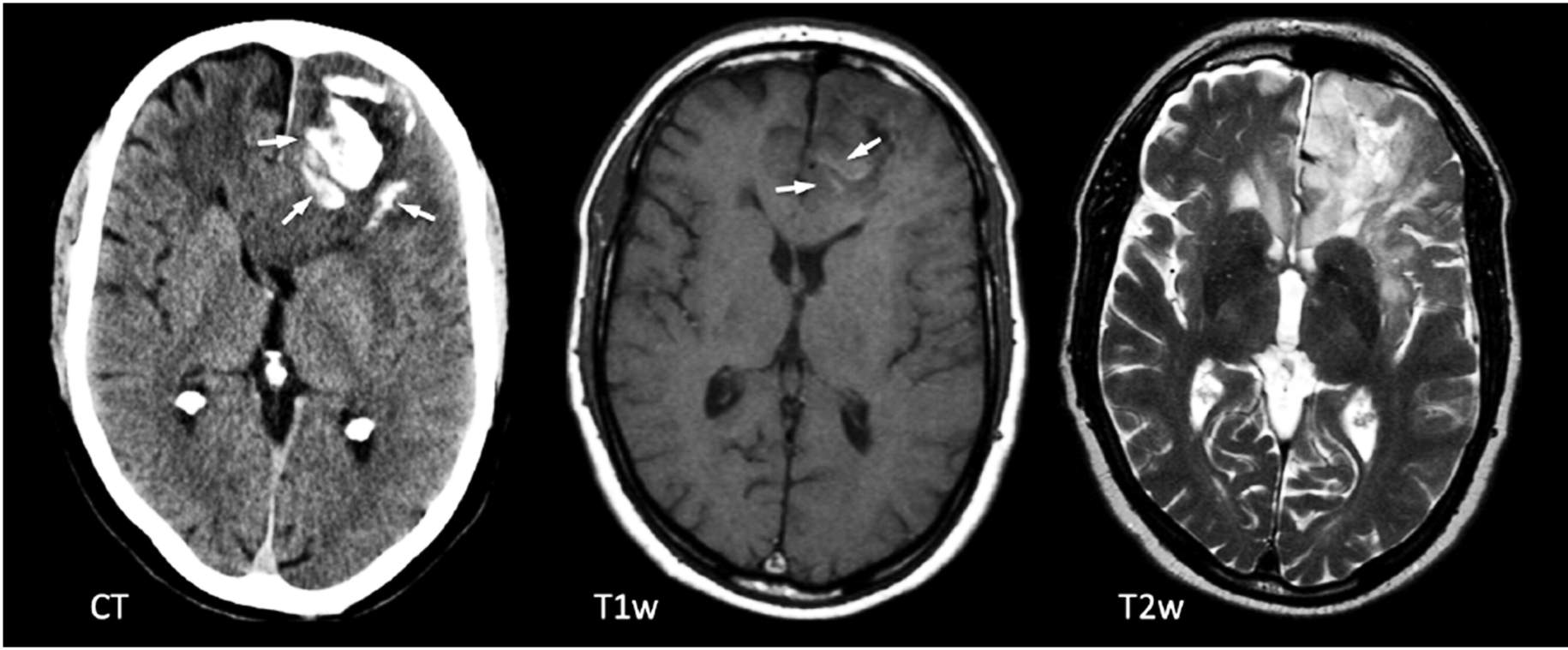
Figure 1: CT (left) and MRI (right 2 images) show calcifications (arrows) on CT in the left frontal lobe, very characteristic of an oligodendroglioma.
What Is Oligodendroglioma?
Oligodendrogliomas are masses, or tumors, caused by overgrowth of certain cells, called oligodendrocytes, primarily in the brain. Oligodendrocytes are cells that form insulation sheaths around nerve cells in the central nervous system (brain and spinal cord). This insulation occurs with a substance called myelin, which helps to increase the speed at which signals transmit along nerves.
What Are the Signs and Symptoms of Oligodendroglioma?
Seizure is the most common presenting symptom for patients with oligodendrogliomas. Many patients may have a history of seizures for several years prior to the diagnosis. Other symptoms are often associated with the tumor pressing on certain structures within the brain and include:
- Headaches
- Vertigo
- Nausea and vomiting
- Memory problems
- Personality and behavioral changes
- Speech difficulty
- Difficulty with balance and movement
- Limb weakness
- Numbness and tingling
Is Oligodendroglioma Cancer?
There are two World Health Organization (WHO) grades of oligodendrogliomas: 1) Grade II (low-grade), 2) Grade III (high-grade). Grade II is often slow growing and considered relatively benign. Grade III (anaplastic oligodendroglioma) grows more rapidly and invades surrounding healthy tissue, making it malignant (cancerous).
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
What Causes Oligodendroglioma?
Like most types of tumors, oligodendroglioma is believed to be caused by abnormal genes within the tumor cells. It is not clear how these abnormalities arise, although ionizing radiation has been implicated. A family history of oligodendroglioma can double the risk of a diagnosis. Most patients are 35 to 44 years of age at diagnosis. These tumors are rare in children. They are more commonly found in men than women.
What Are the Survival Rates?
Overall, approximately 75% of patients are surviving with oligodendroglioma after 5 years. Several factors affect the prognosis for each individual. These factors include the grade of the tumor, other tumor features related to the growth rate of the tumor that are visible with inspection of a biopsy specimen under the microscope, the patient’s age and general health at diagnosis, and the response to treatment. The extent of removal during surgery is also important in prognosis.
How Is Oligodendroglioma Diagnosed?
After a comprehensive history and physical examination, imaging of the brain and spinal cord can identify potential tumors. Computerized tomography (CT) scans and magnetic resonance imaging (MRI) are often used to identify the size and location of the tumor. CT scans use a series of x-rays to create a multi-dimensional image of the brain. MRI uses magnetic fields instead of radiation to create a similar image for evaluation.
Other imaging studies may be necessary if recurrent tumor is suspected, and radiation change versus true tumor needs to be diagnosed.
How Is Oligodendroglioma Treated?
- Surgery is the first and most valuable treatment option, particularly when a tumor is pushing on the parts of the brain and causing symptoms. In patients without symptoms, surgery also improves overall survival. Care is taken to avoid damage to nearby structures during surgery, and minimize the risk of complications.
- Most oligodendrogliomas respond well to chemotherapy. Examples of a common oral chemotherapy regimen includes a combination of:
- Matulane (procarbazine) slows down synthesis of DNA, RNA, and protein in tumor cells.
- Gleostine (lomustine) blocks DNA replication in tumor cells and prevents new cell division.
- Oncovin (vincristine) prevents tumor cell replication and causes tumor cell death.
- Temodar (temozolomide) can be given orally or intravenously. It works by binding to DNA causing tumor cell destruction. Temozolomide may be particularly useful in high-grade and recurrent oligodendrogliomas.
- Efficacy of radiation therapy is still under evaluation but may also provide some advantage. Side effects associated with radiation therapy, including potential damage to nearby structures, must be carefully considered.
Treatment strategies for oligodendrogliomas can be complex. These plans are often highly individualized and crafted by a comprehensive care team comprised of representatives from neurosurgery, oncology, and neurology.











