Meningioma Surgery: Success Rates, Risks, Recovery, and Post-Surgical Expectations

Meningiomas are typically slow-growing tumors originating from the meninges, the membranes surrounding the brain and spinal cord. While most meningiomas grow slowly and may not immediately cause severe symptoms, their growth, location, and size can eventually lead to significant neurological issues.
When a meningioma causes symptoms or starts to grow, surgery is often recommended to remove the tumor. If you have been recommended for meningioma surgery, it’s normal to be anxious about the procedure and what its post-op recovery looks like.
Learning what surgery for meningioma entails, its risks and success rates, and what to expect after it can not only ease your worries but also empower you to make informed health decisions.
What Does a Meningioma Surgery Entail?
As a central nervous system (CNS) tumor, meningiomas growing in specific locations can cause severe symptoms. A growing tumor pressing on important nerves and structures in the brain can even eventually become life-threatening, making treatment necessary.
Your treatment will depend on your overall health and preferences, the tumor’s type and grade, and its location.
In most cases, surgery is used – and is often the only treatment necessary – to treat patients with a benign (noncancerous) tumor that can be completely removed in surgery.
If surgery cannot fully remove a meningioma, the treatment plan also includes radiation therapy and/or chemotherapy to destroy the remaining tumor cells.
What Happens in Meningioma Surgery?
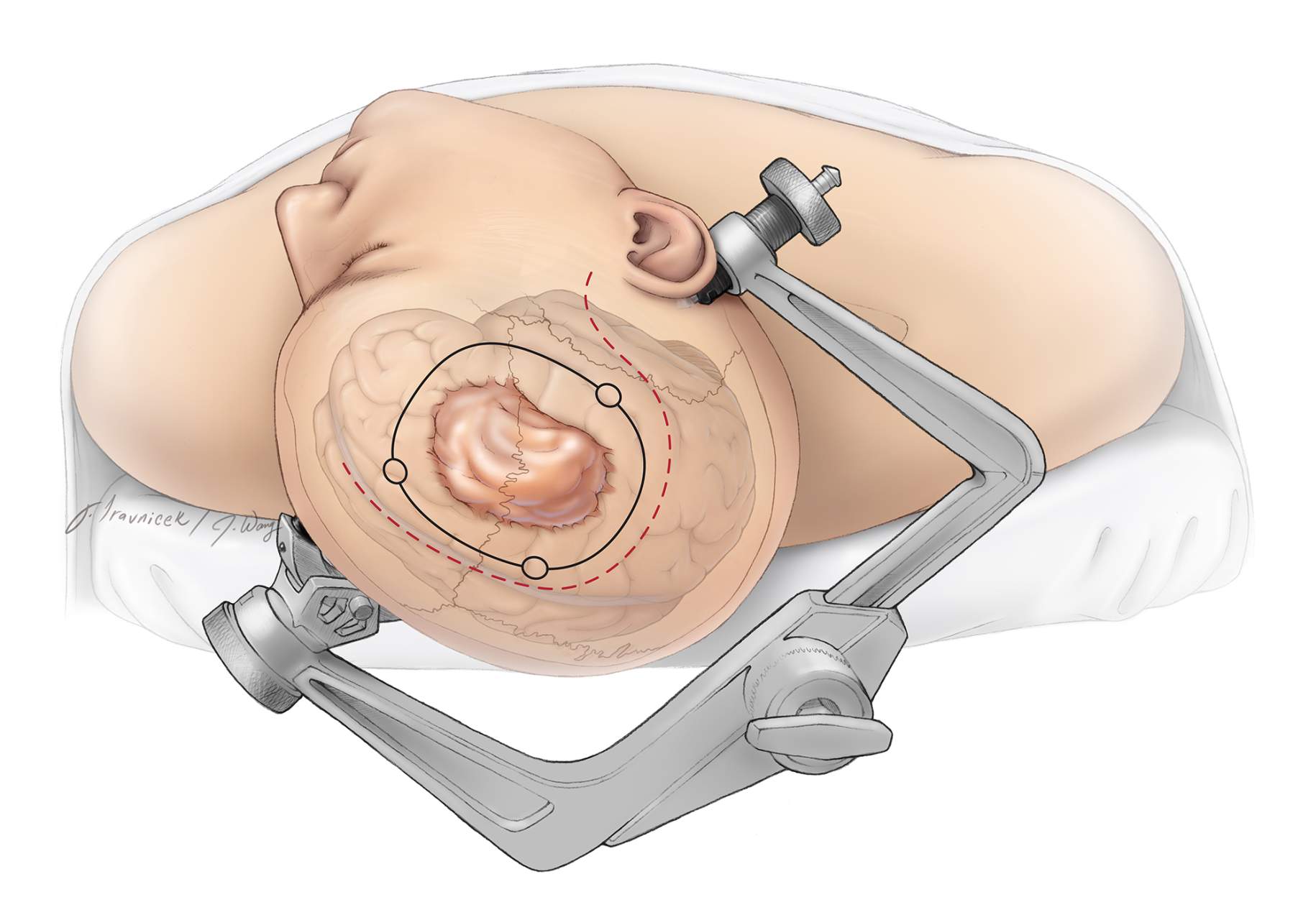
During surgery, neurosurgeons make an incision in the scalp and create an opening in the skull during a procedure called craniotomy to access the meningioma. They then carefully separate the tumor from the surrounding brain tissue or spinal cord. The aim is to remove as much of the meningioma as possible while avoiding any injury to the surrounding structures and therefore preserving neurological function.
Once the tumor has been removed, the patient’s own skull bone or synthetic material will be used to cover the opening of the skull. After the procedure, patients are closely monitored in a recovery room or a specialized neurosurgical intensive care unit.
Because meningiomas are slow to grow and spread, it’s possible to remove an entire tumor safely in many instances. Further treatment may not be necessary after a complete resection.
With all that said, this is a general overview of what happens in surgery for meningioma. It’s best to talk to your neurosurgeon about the specific technique to be used in your procedure, its possible risks, and what you can expect during your meningioma surgery recovery.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Surgery Success Rates and Risks
The survival rate for meningiomas is generally higher than most other types of brain tumors. The 5-year survival rate for patients with benign (noncancerous) meningiomas aged 14 years old and below is at least 95%, 91% for patients between 15 to 39 years old, and 87% for those aged 40 years old and above.
Meanwhile, the 5-year and 10-year survival rates for those diagnosed with malignant meningiomas are at least 66% and 59%, respectively. While these figures are based on five and ten-year periods, it’s worth noting that many patients diagnosed with meningioma live on for decades.
However, like any major surgery, meningioma removal carries standard surgical risks such as infection, bleeding, blood clots, and reactions to anesthesia. Due to the sensitive nature of brain surgery, it may also cause these side effects in rare occasions:
- Seizures
- Stroke
- Difficulty speaking
- Vision problems
- Loss of coordination
- Lack of balance
- Short-term or long-term memory loss
The good news is that most of these side effects are rare and temporary. Moreover, they can be treated through rehabilitation therapy and other methods, so you can remain hopeful for more full and fruitful years after your surgery.
It’s crucial that you find an experienced neurosurgeon for a safe and successful procedure. Seeking a second opinion can also help you further understand the possible outcomes of your meningioma treatment so you can make the best decision for your healing journey.
What To Expect Right After Surgery for Meningioma
Immediately after surgery, patients typically remain in the hospital for monitoring. During this time, your doctor will monitor you for signs of complications, such as infection or bleeding, and manage pain.
The length of your hospitalization will vary based on the complexity of the surgery, your overall health, and any complications during surgery. This could range from a few days to a week or more.
Physical and occupational therapies may begin as early as the day after surgery to assess your ability to perform daily tasks and establish recovery goals.
Upon discharge, your recovery should continue at home.
Short-Term Recovery (Up to 3 Months)
This period is focused mainly on wound healing, diminishing fatigue, and the gradual resumption of physical activities. You may experience cognitive changes and emotional ups and downs during this time, making support from healthcare professionals crucial.
Long-Term Recovery (3 Months and Beyond)
Long-term recovery generally involves various therapies to restore cognitive function, balance, and coordination. Depending on the surgery’s extent and impact, this phase may also involve understanding and coming to terms with any long-lasting changes to brain function.
Surgery Recovery and Adjusting to Life After Surgery
Recovering from your meningioma surgery goes beyond the initial treatment phase and extends into your long-term commitment to your wellness. Whether you underwent surgery or received further forms of intervention, you and your caregiver play a vital role in catching potential signs of recurrence early.
You may need to come in for appointments every 6 to 12 months the first year after your treatment. In these visits, you will undergo neurological examinations and brain imaging studies to monitor for tumor recurrence or growth.
You may also undergo cognitive and psychological assessments to evaluate any changes in your mental function after the surgery.
If these visits show no signs of tumor recurrence and you are stable, the interval between your appointments during the second year onward may be extended. Neurological assessments and imaging studies are typically done during these visits, along with addressing any long-term effects of your meningioma surgery.
Beyond your second year, you might continue to have check-ups at least every two years. These visits often continue for many years to detect late recurrences or new tumors early.
What can you expect during meningioma surgery recovery?
Meningioma surgery recovery looks different for each patient, but many are able to return to a normal and fulfilling life. Successful removal of the tumor often brings significant relief from symptoms such as headaches or neurological issues, leading to an improved quality of life. While some people may experience ongoing challenges like fatigue, memory changes, or emotional adjustments, these can often be managed with rehabilitation and support.
Regular follow-up appointments and brain imaging remain important to monitor for recurrence and address any complications early. Overall, the outlook is highly positive, especially for benign (grade 1) meningiomas, making a full return to daily activities possible for most patients.
Key Takeaways
Meningioma surgery can be a complex and daunting procedure. However, with the right neurosurgeon and a thorough understanding of the risks and meningioma surgery recovery process, it’s possible to achieve a successful outcome.
Finding an experienced neurosurgeon who can perform the surgery safely and effectively is crucial in getting the best outcome. Taking the time to research and seek professional advice can make all the difference in your healing journey.











