Surgical Management of Acoustic Neuromas: What Are Three Main Types of Craniotomies?


Acoustic neuromas, also known as vestibular schwannomas, are benign brain tumors found on the vestibulocochlear nerve, which runs from the inner ear to the brain. The vestibulocochlear nerve is responsible for hearing and balance.
Although acoustic neuromas account for as few as 8 in 100 brain tumors and are benign (non-cancerous), this rare brain tumor type and its treatment can cause challenging symptoms over time, therefore, requiring careful management.
If your neurosurgeon has recommended surgery for your acoustic neuroma, you need to find out which surgical procedure you will receive, what the risks and benefits are, and how your life may be affected in the weeks, months, and years after surgery.
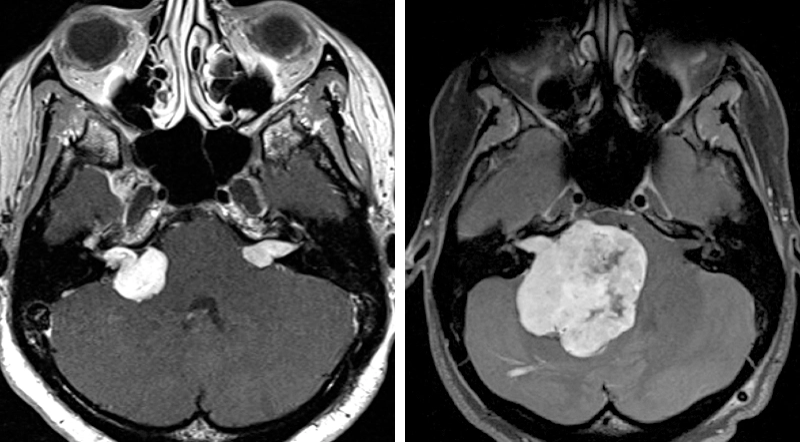
Figure 1: Magnetic resonance imaging (MRI) showing acoustic neuromas of various sizes are shown. Note the difference in small, medium (left), and giant sizes (right).
Treatment for Acoustic Neuroma
If left untreated, acoustic neuromas may eventually grow large, placing pressure on areas of the brain responsible for balance, hearing, and facial expressions.
Because these tumors are benign and slow-growing, if the tumor is relatively asymptomatic, your surgeon may manage your tumor with careful observation over a period of months or years.
When direct treatment is necessary, acoustic neuromas are commonly managed with surgery, although there are other effective treatments available that involve radiation therapy.
In this article, we’ll address the most common surgical approaches used when removing acoustic neuromas.
Surgical Teams for Acoustic Neuroma
Because of their location and involvement with hearing, balance, and other critical functions, acoustic neuromas require a multi-disciplinary team of specialists.
If you are diagnosed with an acoustic neuroma, your surgical team may include a neurosurgeon and otolaryngologist (ear, nose and throat surgeon; ENT) who has received special training in skull base surgery and otology, the study of the ear.
At most institutions, the neurosurgeon and ENT specialists work together to remove the tumor during surgery.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Types of Surgery
There are three main surgical approaches to remove an acoustic neuroma: 1) the retrosigmoid approach; 2) the middle fossa approach; and 3) the translabyrinthine approach. The top qualified surgeons who perform skull base surgery to remove acoustic neuromas are familiar with each of these types of surgical approaches.
They will decide which surgical approach is best for you based on the tumor's size and location, the amount of hearing you have before the operation, and whether or not your hearing can be preserved.
The Retrosigmoid Approach
A retrosigmoid approach, also known as the retromastoid approach, allows the surgeon to remove tumors of different sizes. It is one of the two types of acoustic neuroma surgeries that may allow patients to keep their hearing. The surgeon accesses the acoustic neuroma through an incision and bone opening behind the ear.
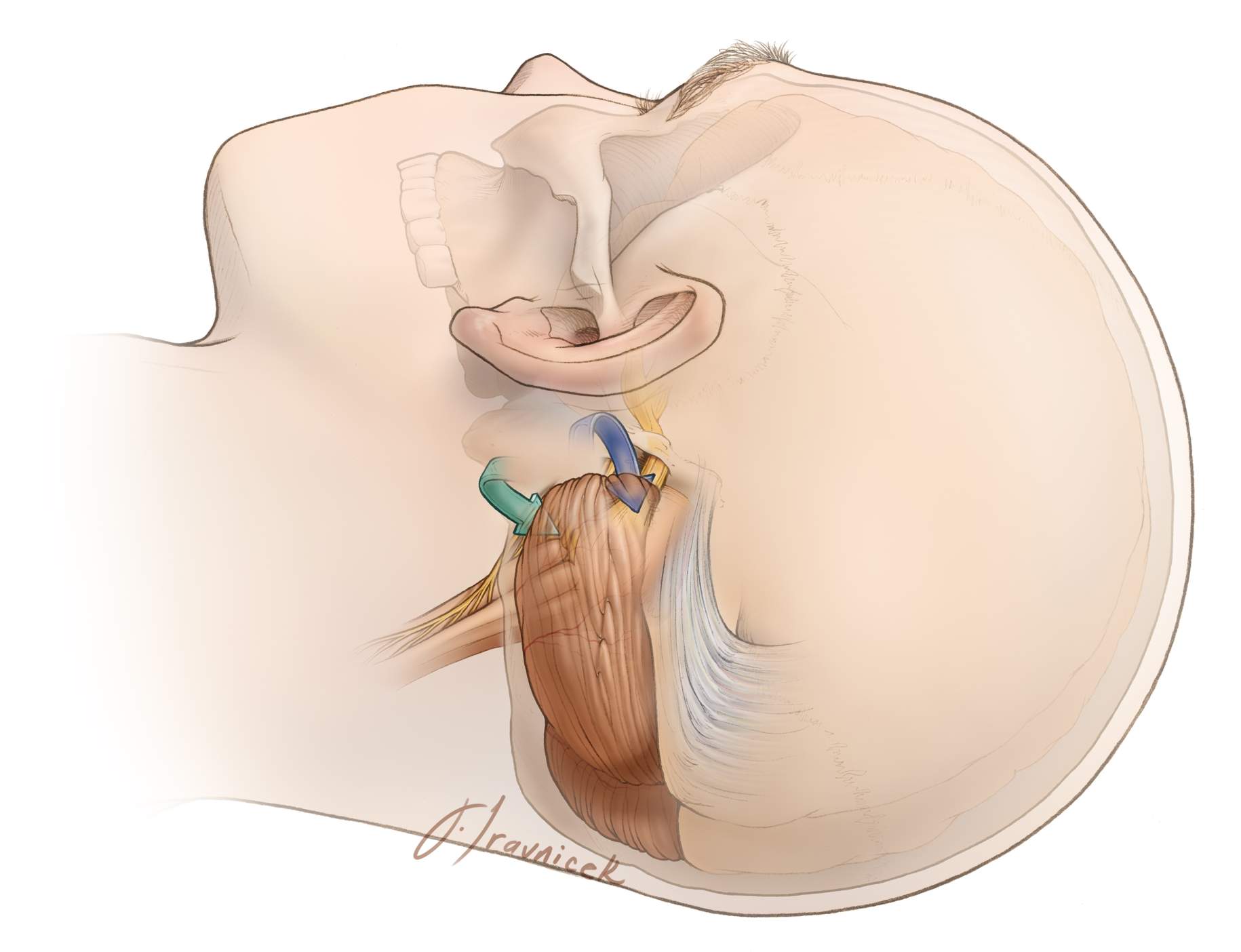
Figure 2: Operative corridors (blue and green arrows) provided by the retrosigmoid approach.
When a surgeon uses the retrosigmoid approach, he or she has a wide view of the tumor and has good access to the entirety of the acoustic nerve. Patients undergoing this type of craniotomy may still have facial movement and hearing after having surgery.
The size of the tumor and its adherence to the facial nerve will determine the outcome of the operation regarding the function of the facial nerve and hearing.
Hearing preservation is possible with small tumors but almost impossible in larger tumors.
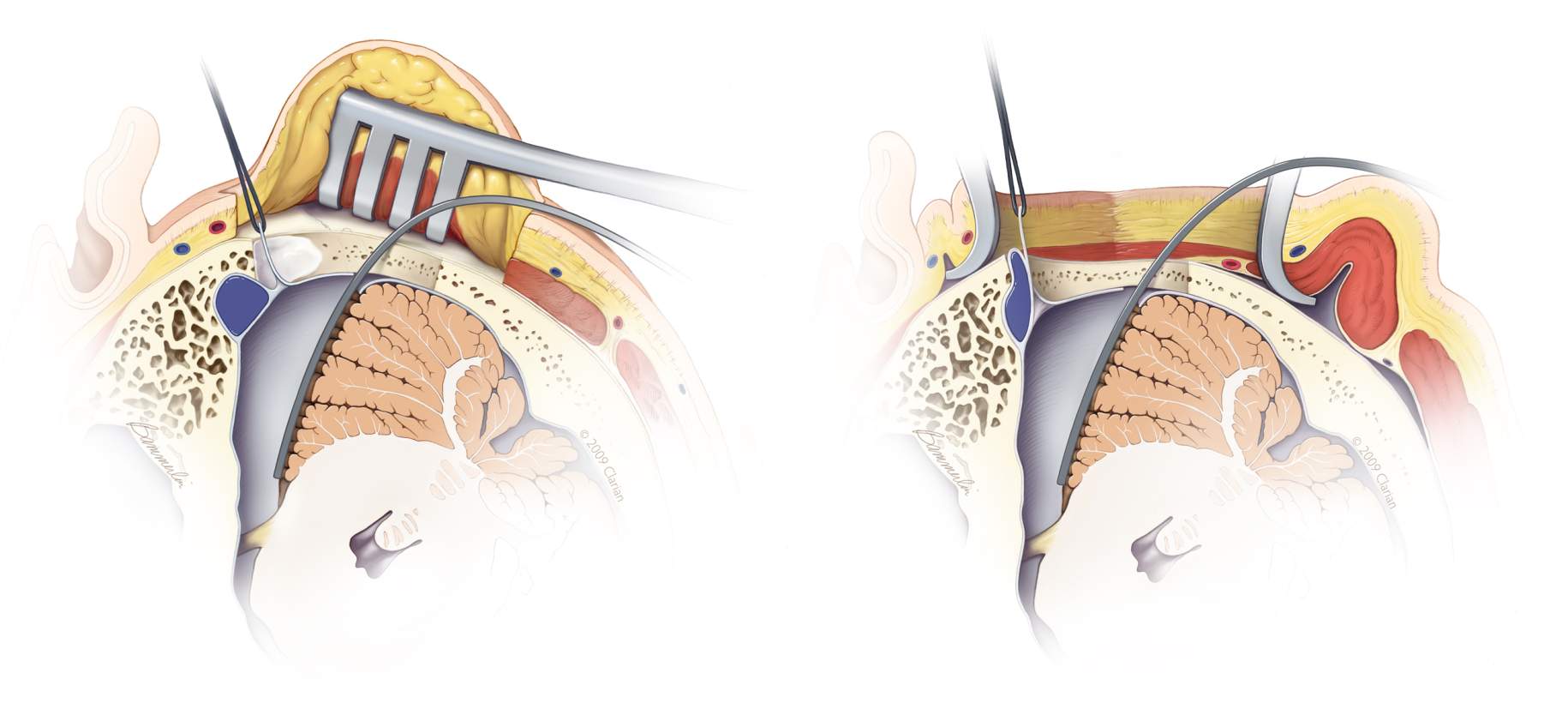
Figure 3: Gentle cerebellar mobilization is required to visualize the entirely of the tumor during surgery.
Just like other types of surgeries for removal of this tumor type, there are some disadvantages to this technique.
The surgeon may have limited access to the facial and cochlear nerves in some regions of the internal auditory canal or ear canal, the corridor that runs between the brain and the inner ear, which may prevent all of the tumor from being removed.
Despite these disadvantages, the retrosigmoid approach is a very common and effective method for accessing acoustic neuromas.
The Middle Fossa Approach
The middle fossa craniotomy is another approach that may be used to preserve the patient's hearing. The surgeon performs a middle fossa craniotomy by making an incision and craniotomy above the ear.
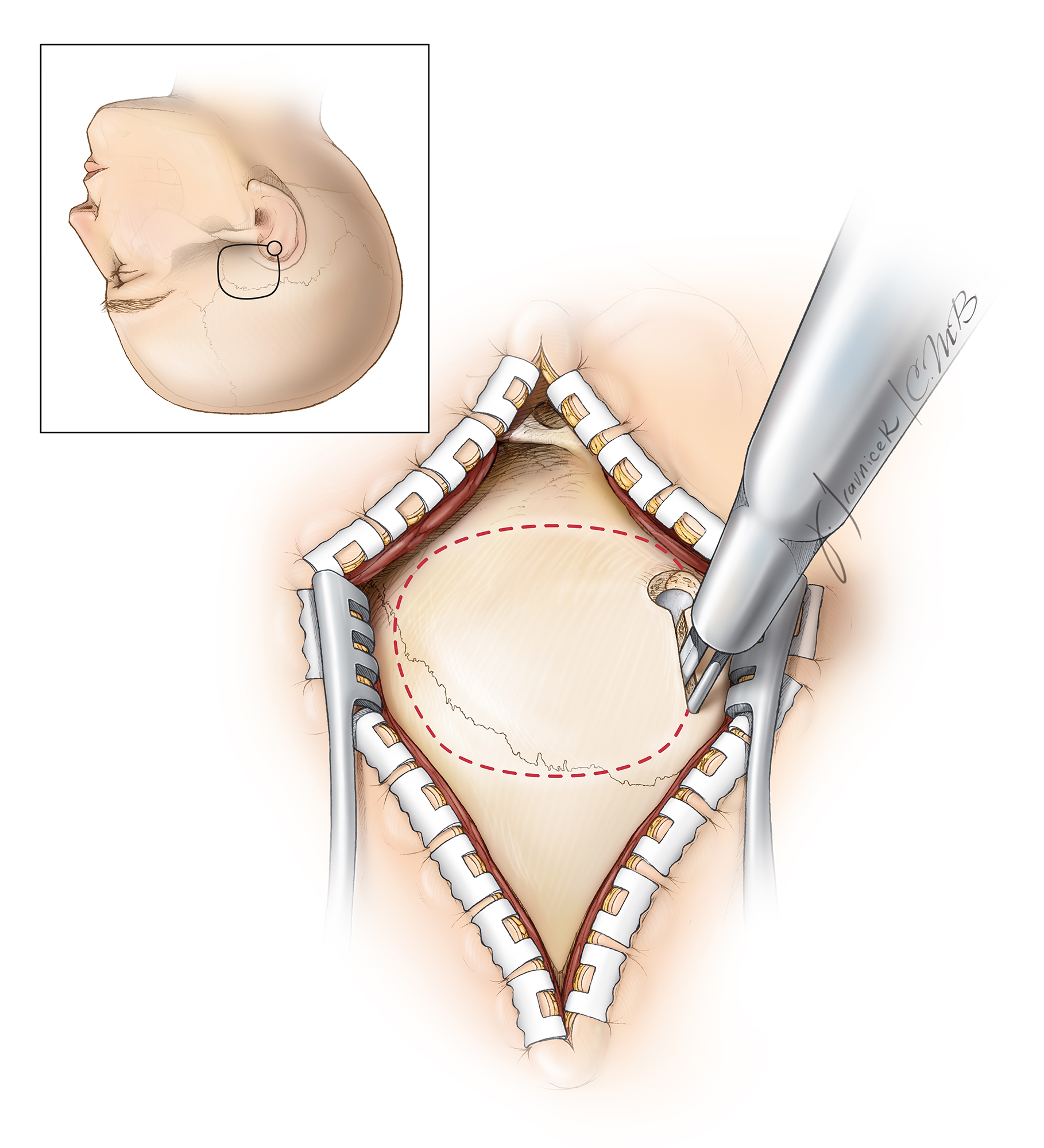
Figure 4: The location of the incision and craniotomy of the middle fossa approach is depicted here.
This approach is optimal with smaller tumors found mostly within the internal auditory canal. When approaching the tumor via the middle fossa, the surgeon has excellent access to the lateral (side) aspect of the internal auditory canal.
This approach maintains the integrity of the dura (the protective covering of the brain) during most of the operation, which avoids unnecessary injury to the underlying brain tissue.

Figure 5: The middle fossa approach allows excellent visualization of acoustic neuromas extending laterally toward the ear.
The Translabyrinthine Approach
For a translabyrinthine craniotomy, the surgeon makes an incision behind the ear as well. Some of the inner ear bone must be removed during the procedure to reach the tumor.
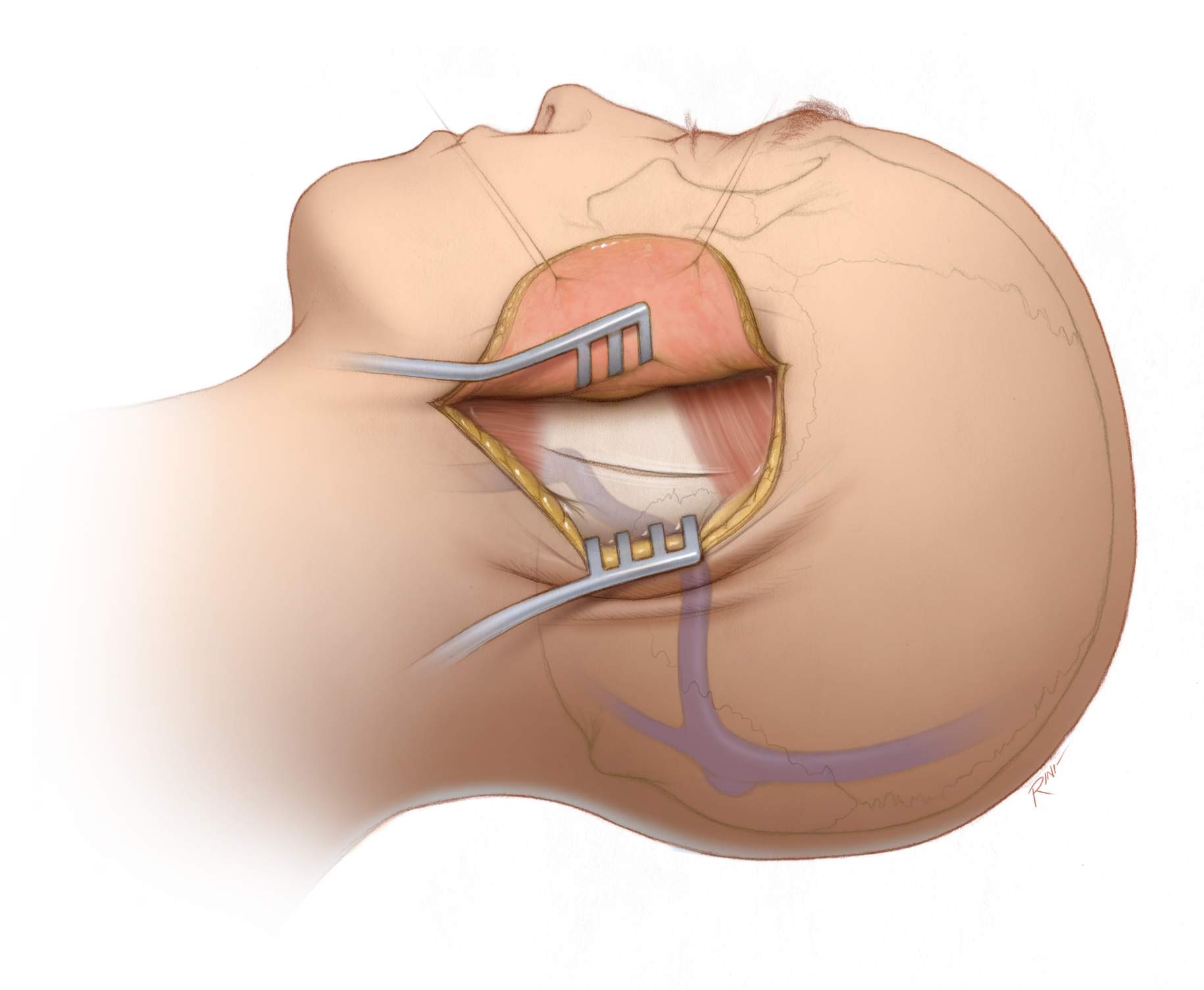
Figure 6: Incision and craniotomy for the translabyrinthine approach.
This approach is commonly used when the patient has little or no hearing before the time of the surgery and involves removing the tumor from the internal auditory canal, the corridor that runs through the inner ear.
Surgical candidates for this approach are also those patients who have large tumors, even if one of the other surgical approaches described above were used previously.
Other advantages of the translabyrinthine approach includes:
- The surgeon can usually use this approach regardless of how large the tumor is.
- The surgical team will be able to find and identify the facial nerve in the auditory canal relatively early and protect it.
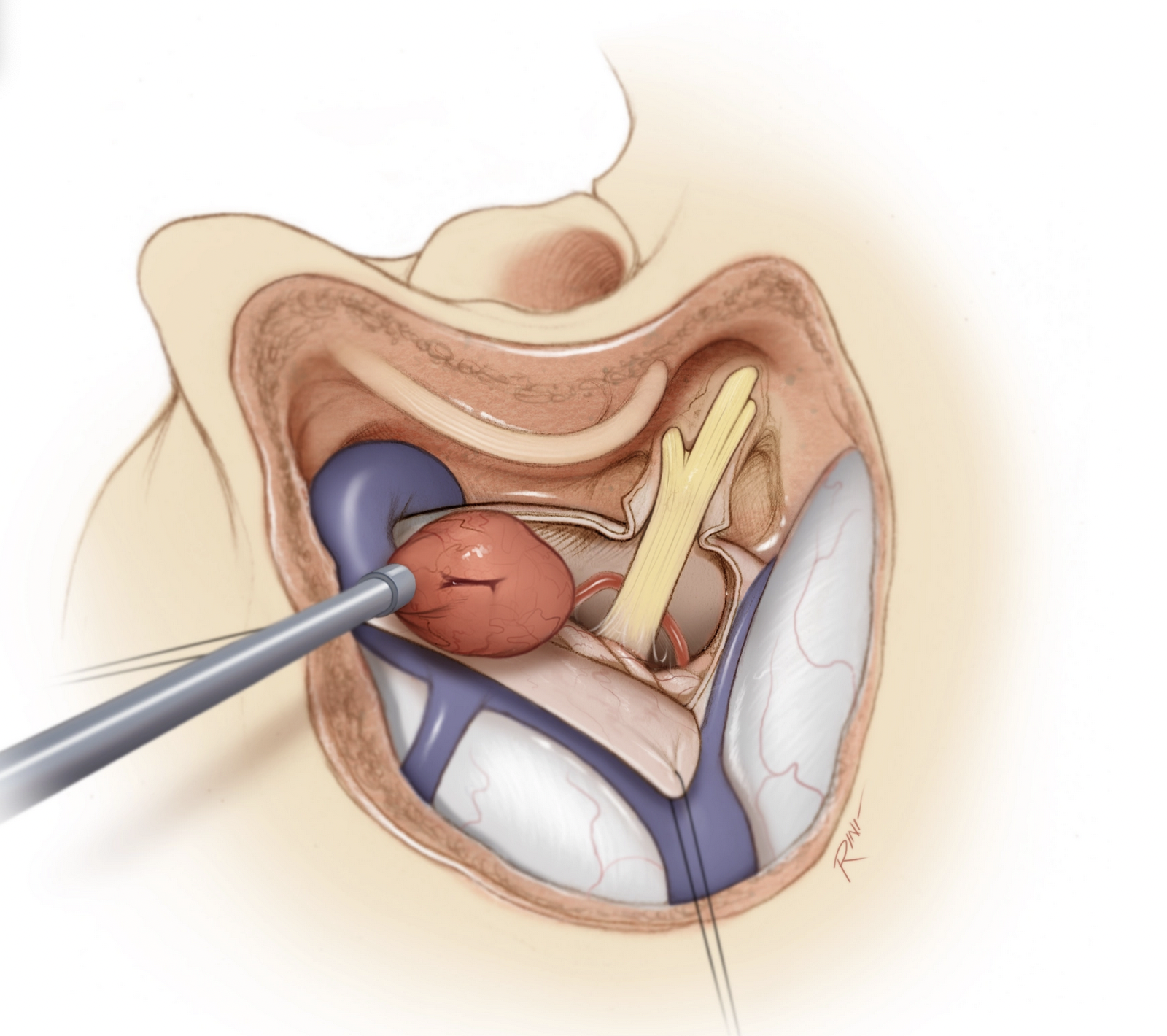
Figure 7: Tumor resection using the translabyrinthine approach.
What to Expect During Acoustic Neuroma Surgery
During acoustic neuroma surgery, patients are placed under general anesthesia, ensuring they are completely asleep and feel no pain throughout the procedure. The specific steps of the surgery will depend on the chosen approach.
However, the following are common elements you can expect during surgery:
- Preparation: The patient's head is carefully positioned, and hair may be shaved at the incision site to reduce infection risk. The area is cleaned, and sterile drapes are applied.
- Incision and Exposure: For each approach, a skin incision is made near the target area. The skull bone is then drilled to create a small window that provides access to the tumor.
- Tumor Removal: The delicate removal of the tumor requires meticulous care to avoid damage to nearby nerves and brain tissue. The goal is to remove as much of the tumor as possible while preserving neurological function.
- Closure: Once the tumor has been adequately removed, the bone window may be covered with a plate and screws, and the skin incision is closed with sutures or staples. A dressing is applied to protect the area.
- Monitoring: Throughout the surgery, the patient's vital signs, brain activity, and nerve function are closely monitored to ensure safety. Techniques such as intraoperative nerve monitoring can help reduce the risk of nerve damage.
The duration of the surgery for acoustic neuroma can vary widely, often lasting several hours, depending on the tumor's size and complexity.
What to Expect After Acoustic Neuroma Surgery: Recovery and Prognosis
Depending on the size of the tumor, surgery is long and usually lasts about 5-8 hours.
- Immediately after the operation: You may feel headache, dizziness, and nausea, and can expect a hospital stay of at least 2 or 3 days. When you are eventually discharged, you will receive discharge instructions that you need to follow carefully.
You will need a family member or other caretaker to drive you home and possibly assist in caring for you over the recuperation period which can last for about 1 month. Typically, your nurse coordinator will brief you extensively on what exactly to expect after surgery.
- Driving: Some patients resume driving a few weeks after surgery, but it varies from patient to patient, depending upon how long it takes to recover your balance during the recuperation period. If you are taking narcotic pain medicines, you should not drive.
- Hearing loss: If the patient had hearing before the operation but is no longer able to hear afterward, the patient should consult with the nurse coordinator and other professionals (ENT specialist) on how to adapt to this lifestyle change.
- Facial weakness and/or facial paralysis: Facial weakness is not uncommon after surgery for acoustic neuromas. Usually it is not permanent and is temporary. You could experience temporary facial weakness or paralysis for six to 12 months after surgery. In some rare instances, facial muscle weakness due to nerve injury may be permanent.
Ask your doctor during your consultation before scheduling surgery about what the likelihood of permanent facial weakness or paralysis will be in your case. This is a major risk of the surgery and depends on the size of the tumor. Larger tumors adhere more significantly to the nerve and place the nerve at more risk during surgery.
Additional procedures may be needed after tumor surgery if facial nerve paralysis is present including placement of a gold weight in your eye lid to allow eye closure and protection of your eye.
Because acoustic neuromas are almost never malignant, operating on them is rarely an emergency. As a result, there will usually be time for you and your family to become fully informed about what to expect during and after your surgery, which type of craniotomy your doctor recommends, and what the benefits and risks are.
Please consult with a radiation oncologist to make sure your tumor is not amenable to radiation therapy as this is another viable and effective method for tumor control and is associated with less risks than surgery.
You should receive as much information as possible so that after surgery you will be prepared for any lifestyle changes that occur.
Discuss with your care team about what improvements to expect in the weeks and months after surgery and which symptoms originally caused by the tumor's presence or surgery will go away, resulting in an overall improved quality of life.
Possible Risks and Complications
As with any surgical procedure, especially one as complex as acoustic neuroma surgery, there are potential risks and complications involved. These can vary based on the surgical approach used, the size and location of the tumor, and the patient's overall health.
Common acoustic neuroma surgery risks and complications include:
- Hearing Loss: Even with efforts to preserve hearing, there is a risk of partial or complete hearing loss in the affected ear, especially if the tumor is large or the surgery involves the translabyrinthine approach.
- Facial Nerve Damage: Damage to the facial nerve can result in temporary or permanent facial weakness or paralysis.
- Balance Problems: As the tumor affects the vestibulocochlear nerve, which is involved in balance, patients may experience balance issues both before and after surgery. These issues usually improve over time but can be permanent in some cases.
- Cerebrospinal Fluid Leak: One of the side effects of acoustic neuroma surgery is the risk of cerebrospinal fluid leaking from the surgical site. This can lead to meningitis, a potentially life-threatening infection of the membranes covering the brain and spinal cord.
- Headache and Pain: Post-surgical headaches and pain are common but usually manageable with medication.
Key Takeaways
- Surgery is the most common treatment method for symptomatic acoustic neuromas. Radiation is another effective option in select small tumors.
- A comprehensive surgical team including a neurosurgeon, and often an otologist, ensures you have the best surgical and post-operative care.
- There are many surgical approaches used for the resection of acoustic neuromas; each with its own advantages and drawbacks. Experienced surgeons will be able to determine the best approach for your situation.











