What Is Cavernous Malformation?
Blood vessels are essential pipelines that transport oxygen and nutrients throughout our body. Abnormalities in the structure of these blood vessels can impair blood flow and disturb normal functioning of surrounding tissues. A cavernous malformation is a rare type of blood vessel abnormality typically spanning a few millimeters to centimeters. Although relatively small, cavernous malformations can cause problems such as seizures and other neurological deficits.
If you or your loved one is diagnosed with a cavernous malformation, it will be important to equip yourself with more information about this rare condition to make informed decisions about your health. Read on to learn more about cavernous malformations.
What Is a Cavernous Malformation?
A cavernous malformation, also known as cavernoma or cavernous angioma, is a berry-like cluster of abnormal blood vessels in the brain that typically spans a few millimeters to centimeters in size. Cavernous malformations lack normal blood vessel walls, becoming leaky and more prone to bleeding. However, blood flow across these lesions is slow, which allows blood to clot.
Cavernous malformations often have multiple lobes or bulges and are composed of a mixture of blood clots in various stages of formation or breakdown, making them look like a mulberry or popcorn on imaging. These lesions are rare and are estimated to occur in 0.3% to 0.5% of the general population. Although most are sporadic, some cases occur in families. Individuals with a familial form of cavernous malformation often have more than one lesion.
Figure 1: Imaging of a cavernous malformation on magnetic resonance imaging with a characteristic “mulberry” or “popcorn” appearance.
Up to 20% of cases of cavernous malformation do not produce symptoms with patients being diagnosed during a magnetic resonance imaging scan (MRI) for an unrelated reason. If a cavernous malformation bleeds, blood breakdown products, particularly iron, can irritate the surrounding brain and contribute to the development of seizures.
The impact of a cavernous malformation can vary widely from person to person. While some may experience no symptoms at all, others may develop seizures that significantly impair daily life. Although all conditions related to the brain are a serious matter, cavernous malformations are not brain tumors or cancer and typically do not affect life expectancy.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,000+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Types of Cavernous Malformations
Cavernous malformations can be sporadic or hereditary. Hereditary forms of cerebral cavernous malformations are associated with mutations in 1 of 3 genes: KRIT1 (CCM1), MGC4607 (CCM2), or PDCD10 (CCM3).
These mutations are passed down in an autosomal dominant manner, which means that children of individuals with the familial form of cerebral cavernous malformation will also inherit this mutation. However, the manifestations between family members can vary widely with some experiencing severe symptoms and others experiencing no symptoms at all.
Symptoms of individuals affected by mutations in CCM1, CCM2, or CCM3 are like that of general symptoms of a cavernous malformation if a cavernous malformation does develop. However, such individuals may have multiple cavernous malformations and experience more frequent and/or severe symptoms.
Difference Between Cavernous Malformations and Arteriovenous Malformations
Like cavernous malformations, an arteriovenous malformation (AVM) is another type of vascular malformation where blood vessels are not formed properly. However, the principal difference is in the pressure and flow of each lesion. Blood flows slowly across the low-pressure cavernous malformation, whereas blood flows rapidly across the high-pressure arteriovenous malformation. Compared with an arteriovenous malformation, cavernous malformations have a lower risk of devastating hemorrhage.
Risks and Symptoms of Cavernous Malformations
Nearly 20% of cavernous malformation patients do not experience any symptoms. These cavernous malformations remain undetected until found incidentally, or unexpectedly, on an imaging test. However, cavernous malformations can cause severe symptoms especially if they are located near critical structures such as the brainstem or basal ganglia. Symptoms of cerebral cavernous malformations can include:
- Headaches
- Seizures
- Muscle weakness
- Issues with memory and cognition
- Balance problems
- Paralysis
- Vision changes
Seizures and headaches are the most commonly reported symptoms. Specific neurological impairments are related to the location of the cavernous malformation, its size, and the integrity of its walls (that is, do the walls appear intact or show any sign of weakness or damage). Because cerebral cavernous malformations are dynamic lesions that can change in size as blood is reabsorbed or accumulates, symptoms may disappear or recur over time.
Risk of Hemorrhage
The risk of hemorrhage among cavernous malformations discovered incidentally is very low, with an estimate of less than 1% per year. This risk is increased to approximately 3% to 5% per year for cavernous malformations that have previously bled or those located in the brainstem. However, because of the slow nature of blood flow, bleeding from a cavernous malformation typically produces less severe neurological impairments than other types of vascular malformations, such as an arteriovenous malformation.
What Is a Cavernous Tumor?
When a cavernous malformation ruptures, it slowly leaks blood into the surrounding area. Sometimes, the blood is reabsorbed by the body. However, it may leave behind breakdown products that can harden and form a shell around the malformation.
This tumor-like mass is sometimes referred to as a cavernous tumor. However, these are not considered actual brain tumors. A brain tumor is a mass of abnormal cells that continuously divide, whereas a cavernous malformation consists of cells that are abnormally arranged. Cavernous malformations may grow because of accumulation of blood and fluid but can also shrink when the blood products are reabsorbed.
Treatment Options for Cavernous Malformations
The optimal treatment option for cavernous malformations will depend on various factors, including your symptoms and the location of the cavernous malformation. For cavernous malformations that do not produce any symptoms, the physician may recommend regular monitoring. Any changes that occur during this observation period may alter the course of treatment.
If you are experiencing symptoms such as seizures, the physician may initially recommend a trial of antiepileptic medications. If medications fail to control seizures or produce intolerable adverse effects, surgical removal may be recommended. Surgery may be considered earlier for cavernous malformations that are closer to the surface to the brain and more easily accessible. Complete surgical removal of the cavernous malformation is currently the most effective approach at controlling persistent seizures but carries inherent risks, especially if the cavernous malformation is located in a deep and/or critical area.
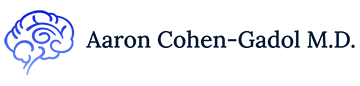
Figure 2: Surgical removal of a cavernous malformation. The brain is gently pulled back, and long instruments are passed through to access the lesion.
If the cavernous malformation resides in a deep location relatively inaccessible by a surgical approach, stereotactic radiosurgery may be rarely recommended. Stereotactic radiosurgery also comes with risks of damaging brain tissues, although it may reduce the bleeding rate after a period of several years. The use of stereotactic radiosurgery for the treatment of cerebral cavernous malformations is still debated.
Key Takeaways
- Cavernous malformations are regions of abnormal leaky blood vessels. They can develop in the brain, brainstem, and spinal cord.
- Some individuals with cerebral cavernous malformations do not experience symptoms, but those who do most commonly report seizures or headaches.
- Treatment options depend on the presence of symptoms and the location of the cavernous malformation.