What Is Arteriovenous Malformation?
An arteriovenous malformation (AVM) is a condition characterized by abnormal connections between an artery and vein. Although this sounds relatively benign, AVMs can lead to a variety of complications. If left untreated, an AVM can rupture, and lead to significant challenges and neurological decline such as memory issues, weakness, and numbness.
Several different types of AVMs can form in and around the brain. Understanding the different types of AVMs and the effects they may cause can provide clarity regarding your diagnosis and treatment options. In this article, we review the different types of AVMs and other vascular malformations.
What Is a Brain AVM?
A brain AVM is an abnormal tangle of blood vessels connecting an artery and vein in or around the brain. To understand what an AVM is and why it causes problems, we must first discuss normal blood flow.
Our heart pumps freshly oxygenated blood throughout our body via strong blood vessels called arteries. Blood flows from arteries to much narrower capillaries (only one cell thick!) which slows the passage of blood to allow for distribution of essential oxygen and nutrients to surrounding tissues. This now oxygen-depleted blood is then delivered to veins that carry blood back to the heart.
In an AVM, an artery is connected directly to a vein without an intervening capillary network. Blood rushes from the high-pressure artery to the low-pressure vein and is unable to transfer oxygen to neighboring tissues. Since this shunt offers less resistance than nearby normal capillaries, blood is also preferentially directed to the AVM and is thus “stolen” from adjacent arteries (steal phenomenon). A lack of oxygen and nutrients will eventually lead to brain tissue damage.
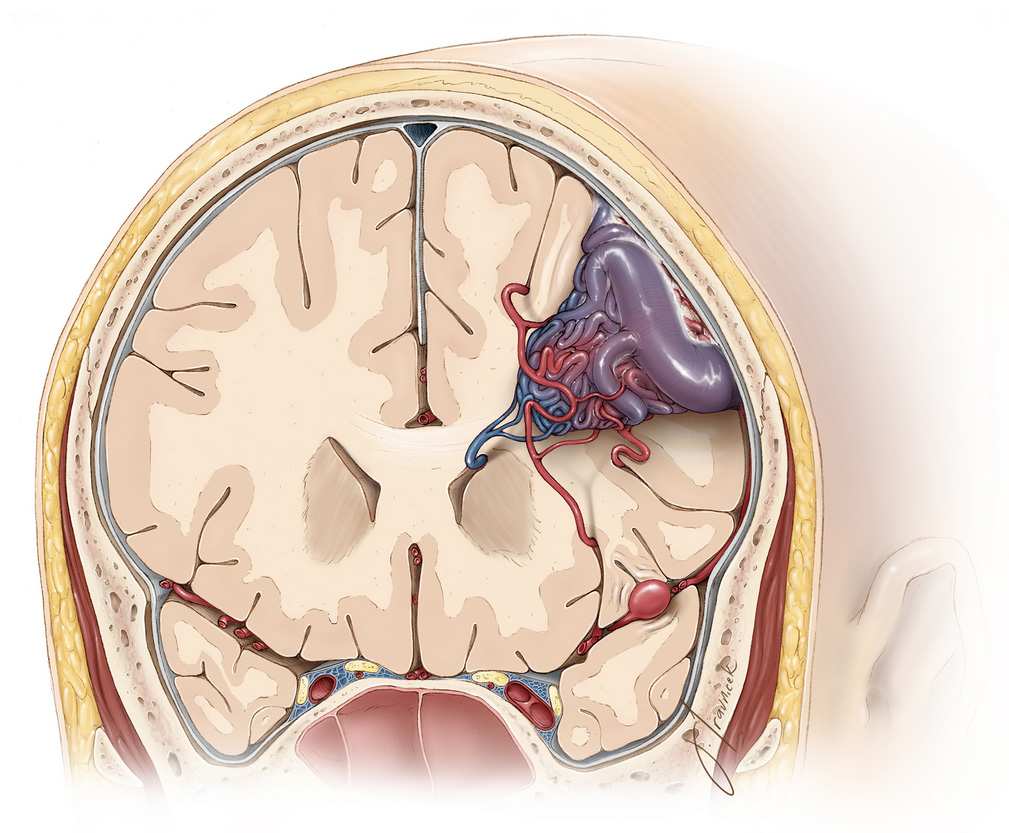
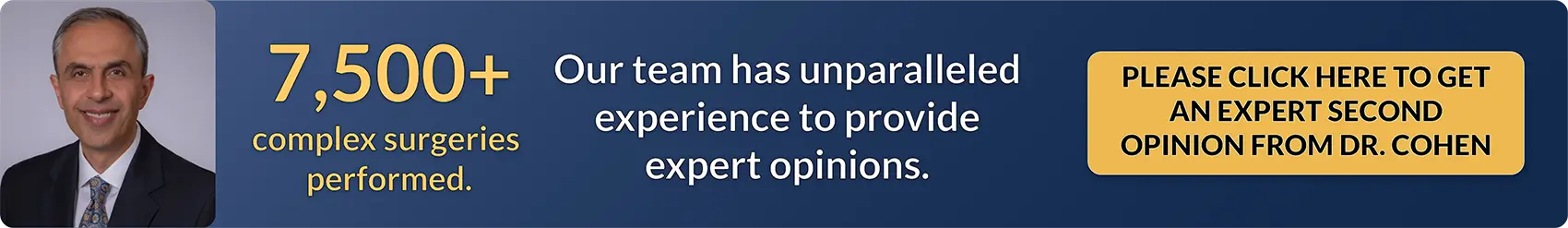
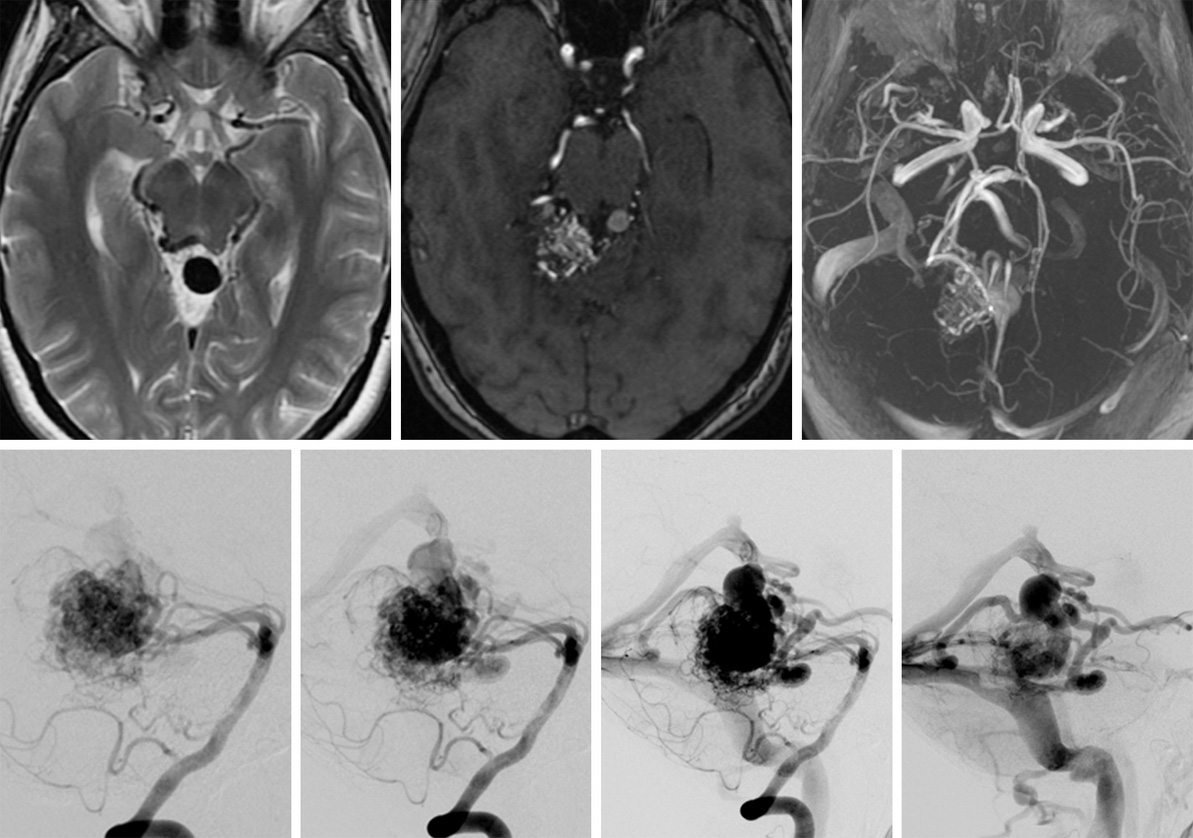
Figure 1: A large AVM with engorged purple veins.
What Makes a Brain AVM Dangerous?
Rapid blood flow from the high-pressure artery to low-pressure vein prevents the brain from receiving adequate amounts of oxygen which can lead to cell death. Additionally, blood rushing from the artery to the thinner-walled vein can cause the vein to become engorged. Over time, constant turbulent blood flow can weaken the walls of the AVM leading to devastating rupture and bleeding within the brain.
Brain hemorrhages, in turn, can cause several complications of varying severity, including:
- Severe and sudden headaches
- Seizures
- Stroke
- Loss of brain function
- Weakness in the arms and legs
Depending on the location and size of the ruptured AVM, rising pressure in the brain due to blood leakage can become fatal if not treated quickly. In rare cases, an AVM can cause damage to your brain before rupture simply by its size. As blood builds up within its tangled vessels, an AVM can enlarge and eventually place pressure on its surroundings.
A sufficiently large AVM can also restrict the flow of cerebrospinal fluid. Cerebrospinal fluid is constantly produced and functions to nourish and protect the brain. With flow blockage, cerebrospinal fluid can accumulate within the brain causing a condition known as hydrocephalus. This can further increase pressure on the brain and cause neurological impairments.
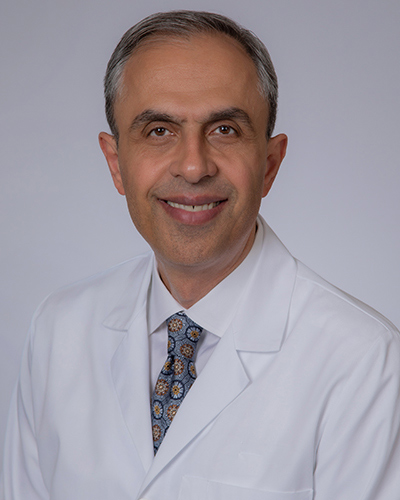
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
What Are the Other Types of AVM?
AVMs can be classified by their general location with parenchymal AVMs found in the brain and dural AVMs in the tough outer membrane (dura) covering the brain and spinal cord. AVMs can be named by the region that they occupy, such as the lobe of brain or a distinct part of the brain like the cerebellum and brainstem. AVMs can also by classified by their Spetzler-Martin grade, which can help to predict the risk and outcomes of surgery.
Location
AVM types by location and the percentage of patients that have each subtype is as follows:
- Frontal AVMs (24%) develop in the frontal lobes of the brain near the forehead.
- Temporal AVMs (19%) develop in the temporal lobes of the brain near the temples.
- Parieto-occipital AVMs (19%) develop in the parietal and occipital lobes of the brain near the top and back of the head.
- Periventricular AVMs (7%) develop near the ventricles, which are fluid-filled cavities deep within the brain.
- Deep AVMs (8%) develop near structures that are at the deep center of the brain.
- Brainstem AVMs (3%) develop in the brainstem connecting your brain to your spinal cord.
- Cerebellar AVMs (20%) develop in the cerebellum at the back and bottom of your head.
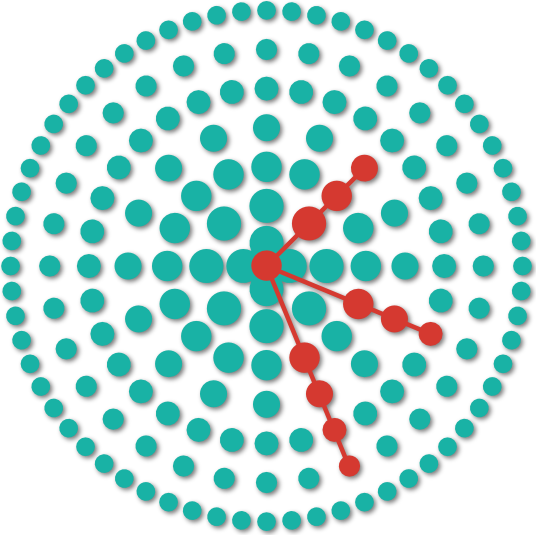
AVMs in the dura are also known as dural arteriovenous fistulas. Dural AVMs more commonly occur near structures called dural venous sinuses (Figure 2).

Figure 2: Common locations of dural AVMs near dural venous sinuses (blue).
Grade
Another way that AVMs can be named is by their grade. This is based on the Spetzler-Martin grading system, which scores an AVM from 1 to 5 by its size, location, and blood drainage pattern. The score corresponds to its grade, with grades I and II often referred to as “low-grade” AVMs and associated with better outcomes after surgery. The scoring is as follows:
Size
The largest diameter of the AVM, which can be measured from imaging tests prior to treatment.
- < 3 cm (+1)
- 3 – 6 cm (+2)
- > 6 cm (+3)
Venous Drainage
Whether the blood vessels draining the AVM are located closer to the surface (superficial drainage) or deeper within the brain (deep drainage).
- Only superficial drainage (+0)
- Deep drainage (+1)
Eloquence
Whether or not an AVM is located within critical brain structures such as areas involved in language, sensation, or movement, and deep structures.
- No (+0)
- Yes (+1)
Other types of vascular malformations include the following:
- Cavernous malformation (aka cavernous hemangioma, cavernoma, cavernous angioma, angioma): Abnormally formed tangle of blood vessels that periodically bleed forming "popcorn-like" or “mulberry” lesions in the brain or rarely in the spinal cord. These lesions have thin walls and can contain blood of varying ages pooled within them. The often cause seizures.
- Developmental venous anomaly (DVA) (aka venous angioma or venous malformation): Abnormally enlarged veins that often do not interfere with the function of blood vessels and rarely hemorrhage. Most do not cause any symptoms.
- Vein of Galen malformation (aka Vein of Galen aneurysm): Severe type of malformation characterized by abnormal enlargement of the great cerebral vein of Galen located deep within the middle of the brain. Newborns with this malformation can present with symptoms such as swollen scalp or facial veins, heart failure, seizures, and enlarged head size soon after birth.
- Capillary telangiectasia: Clusters of swollen capillaries that usually measure less than an inch in diameter. They are rarely large enough to cause damage to the brain or lead to any symptoms, and if they hemorrhage, they do so in microscopic (very small) amounts.

Figure 3: “Popcorn” or “mulberry”-like lesion of a cavernous malformation on imaging.
What Is the Treatment for AVM?
The optimal treatment option depends on the age and overall health of the patient, risk of AVM complications including rupture, symptoms, and factors specific to the AVM itself such as its size and location. Surgery is typically the treatment of choice if treatment is pursued. However, if surgery is too risky, other options such as radiation therapy and/or embolization may be performed. A combination of these therapies may also be used.
Though receiving a diagnosis of an AVM may be disconcerting, not every occurrence of an AVM requires treatment. The risk of AVM rupture if left untreated is approximately 2 – 4% per year. The lifetime likelihood of rupture for an older person with an AVM is less likely than that of a younger person and thus regular monitoring may be recommended.
The risks and benefits of treatment will be weighed against the risks of sustaining complications from an AVM on a case-by-case basis. The main concern for an AVM is the possibility of rupture and bleeding within the brain as this can be life-threatening and cause neurological deficits if not treated promptly. On the flip side, treatment options like surgery come with, albeit small, potential complications such as bleeding during the operation and damage to healthy tissues surrounding the AVM.
Key Takeaways
An arteriovenous malformation (AVM) is a condition that occurs due to abnormal blood vessel connections between an artery and vein. There are different types of AVMs depending on the size and where they form. An AVM that forms in the brain can present with significant risks to your health due to the possibility of rupture and bleeding within the brain. Surgery, endovascular embolization, and radiosurgery are the primary methods of treatment.