Surgery for Craniopharyngioma

Craniopharyngiomas are relatively rare benign tumors of the central nervous system. Their location and intimate association with structures such as the visual pathways, cranial nerves, pituitary gland, hypothalamus, and blood vessels predisposes patients to complex deficits both at presentation and after treatment.
In most cases, the primary treatment is surgery to remove the tumor. The procedure can be performed via either a transcranial approach through an open craniotomy or an endoscopic transnasal transsphenoidal approach.
Surgeries can be technically challenging with increasing difficulty depending on the tumor location, size, invasiveness, and the proximity and tumor adherence of vital nervous and vascular structures. The best approach for surgery is determined by factors unique to the patient, the tumor, and the neurosurgeon's experience. Irrespective of the surgical technique, patients are evaluated and treated individually by multidisciplinary medical teams of endocrinologists, ophthalmologists, otolaryngologists (ENT), internal medicine doctors, and radiation oncologists; this strategy favors the best possible outcomes.
Indications for Surgery
Surgery is typically indicated when the tumor causes neurologic deficits, hormonal alterations, and increased intracranial pressure. The main goal of surgery is safe and complete tumor removal, as well as confirmation of diagnosis. However, this may not be possible if the tumor is in close contact with critical surrounding structures, and the neurosurgeon may instead perform partial removal of the tumor and recommend radiation therapy after surgery. A surgeon’s experience plays an important role in his or her ability to achieve a safe complete tumor resection.
Neurosurgeons evaluate each case individually before determining the amount of tumor to remove. A balance between risks and benefits is what guides the approach and aggressiveness of treatment. Importantly, in pediatric patients, the long-term outcomes of surgery depend on access to socio-economic support, neurological care, and endocrinologic supervision.
Surgical Management Options
The two basic surgical approaches to treat most craniopharyngiomas are the transcranial and the transnasal routes. The selected approach is determined by a detailed evaluation of the tumor size and location, the invasion of adjacent structures, and the neurosurgeon's experience. The transnasal route is minimally invasive and uses the natural nasal entrance to access the tumor. It is particularly effective when the tumor is located at the midline and base of the brain.
The more invasive transcranial route is less commonly used but valuable for larger tumors with a complex shape and location that require wider surgical visualization and operative area for manipulation. Regardless of the technique, the extent of tumor resection is unique to each patient and aims to remove the most amount of tumor while preserving the patient's functional status.
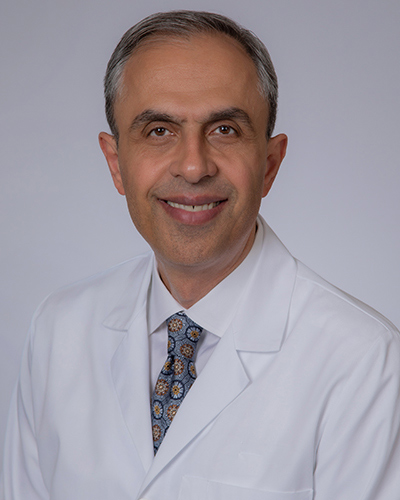
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Preparation for Surgery
A comprehensive pre-operative evaluation of each patient is undertaken in preparation for surgery. Baseline health status, medical history, and imaging studies are reviewed to establish the optimal treatment plan.
Pituitary hormone levels are checked and, if necessary, corrected before starting the procedure. Patients and families are encouraged to ask questions and obtain information to lessen their anxiety by increasing their knowledge about what should be expected.
Transnasal Approach
The transnasal approach is also known as the transsphenoidal approach due to the name of the sinus bone at the back of the nose (i.e., sphenoid bone) that must be crossed to reach the anatomical site where most craniopharyngiomas grow (Figure 1). For this technique, minimally invasive surgical instruments and a camera or microscope are inserted through the nose openings. Commonly, the transnasal approach is performed in conjunction with an otorhinolaryngologist who aids the neurosurgeon during specific stages of the surgery.
When a microscope is used, the surgeon can observe the operative area directly. On the other hand, when the endoscope (i.e., camera) is used, the viewing angles can be adapted to the surgeon's choice. Both options offer valuable advantages for specific cases, but the endoscopic approach allows resection of larger tumors through the nose via the expanded endoscopic transnasal skull base surgery.
In children, a baseline consideration for transsphenoidal surgery is the size and development of the nasal sinuses. For instance, performing transnasal surgery on patients less than 10 years of age can be technically difficult and in some cases an unfavorable option. However, even though specific patient characteristics make this approach challenging, advances in endoscopic techniques and improved surgical equipment have allowed surgeons to expand the feasibility of transsphenoidal surgery to younger children and successfully operate on most tumors located in the midline.
The procedure starts with general anesthesia, positioning of the patient, and cleaning the surgical fields. Next, the equipment (i.e., microscope or endoscopic camera) is inserted through the nose. The first visualized bone at the back of the nose is the sphenoid. After removing a piece of the sphenoid bone, the skull is entered. Several protective tissue layers such as dura are incised, and vital structures such as nerves and blood vessels are identified and preserved. Next, the tumor is visualized and removed totally or partially according to the case. After tumor removal, the surgical area is thoroughly inspected. If no bleeding is identified, closure is performed in layers. The primary goals are to achieve the best surgical outcomes.
The experience of the surgeon in conducting the procedure is very important to secure best outcomes.
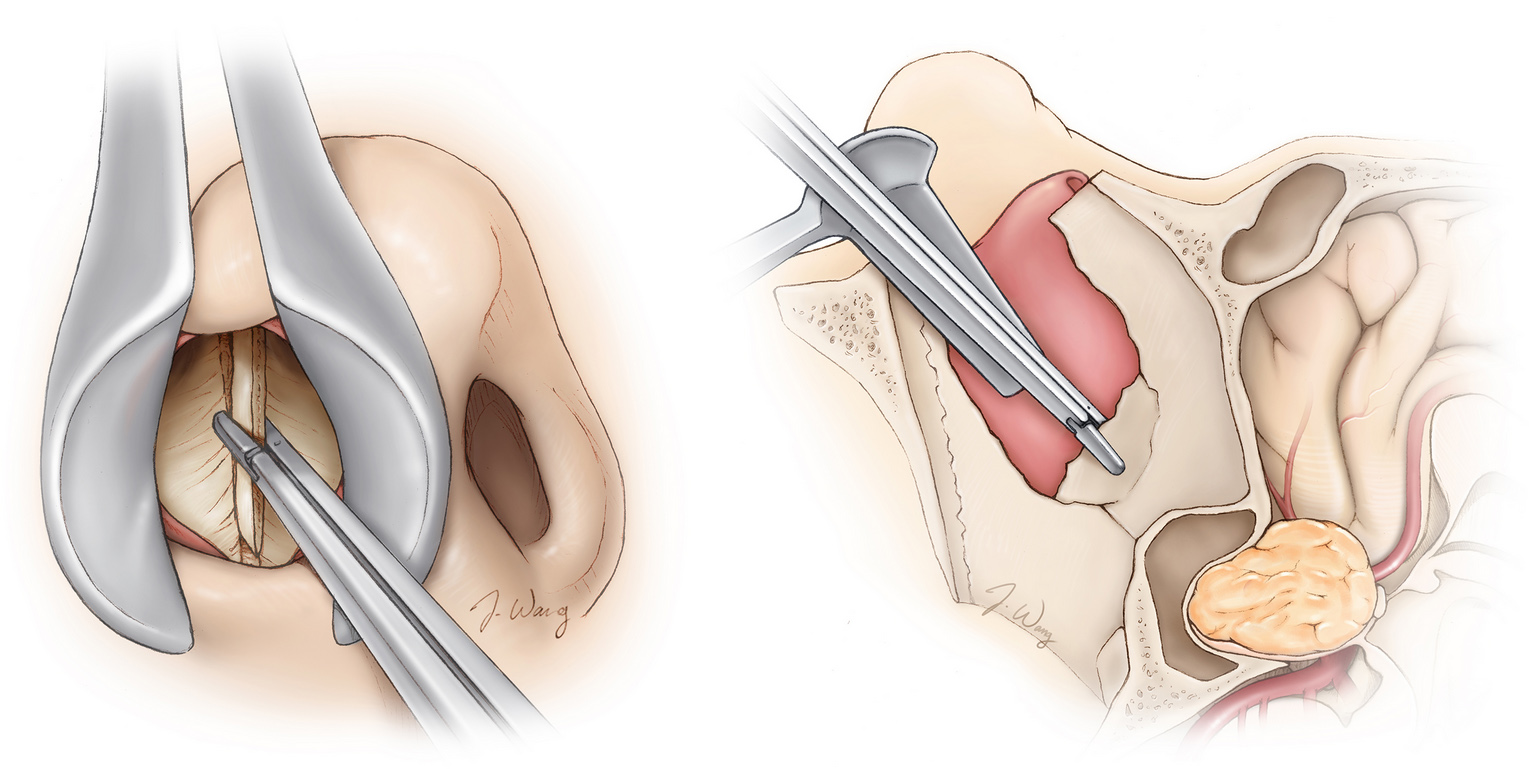
Figure 1. Long surgical instruments are passed through the nose in the transnasal approach.
Transcranial Approach
In contrast to the transnasal approach, the transcranial approach opens the skull to reach the tumor through a procedure called a craniotomy (Figure 2). There are different types of transcranial routes to choose from. The choice to use one route versus another is based on the anatomy of the lesion and the neurosurgeon's preference.
The most common routes are the pterional, frontotemporal or supraorbital, and orbitozygomatic. Their names reflect the bone or location of the entrance to the skull. Each route allows the surgeon to view and operate in a specific area and direction.
The patient first receives anesthesia and is positioned on the surgical table. The scalp is cleaned, and the surgeon creates an incision to reach the bone just behind the hairline. A piece (i.e., bone flap) is removed to enter the skull. Next, the protective coatings of the brain are opened. Once the brain is visualized, the neurosurgeon gently elevates a part of the exposed brain to reach the tumor.
The resection of tumor is done carefully until the desired result is achieved. Before exiting the skull, the surgical field is inspected in detail. If no bleeding or irregularities are found, the surgeon puts back the original bone flap and closes each layer of the scalp.

Figure 2. Craniotomy procedure to open the skull.
Post-operative Care
After surgery, patients are taken to a recovery room and closely monitored while they awake from anesthesia. Nausea and headache are common symptoms after both surgeries. However, nasal congestion is more specific to the transnasal route. In addition, it is relatively common for patients to experience temporary excessive thirst and urination due to hormonal imbalances after surgery.
Blood and hormone tests are performed to evaluate any abnormalities. Medical treatment is offered to control the variations in hormonal levels and manage the pain and swelling associated with the surgery. Excessive urination (diabetes insipidus) is common and is managed medically.
An imaging study is performed to assess the results of surgery and extent of resection. Finally, patients are discharged home with instructions.
Surgical Risks
General surgical risks such as adverse reactions to anesthesia and/or medications, bleeding, infection, and death are present but very rare. A specific risk in craniopharyngioma surgery is the loss of hormonal production by the pituitary gland or the hypothalamus. This risk is higher in cases with large and invasive tumors. However, this can be managed by hormone supplementation and followup with an endocrinologist.
Another relevant complication is the leakage of brain fluid (i.e., cerebrospinal fluid) following the operation. Other complications are damage to the surrounding structures, which can ultimately cause vision loss. Notably, the skills and experience of the surgical team and the surgeon are fundamental to avoid complications.
Outcomes
Around 90% of patients with craniopharyngioma survive at least 10 years following treatment. However, recurrence is relatively common, even after complete removal of the tumor. If a recurrence is detected, repeat surgery and radiation therapy treatments can be used. After treatment, patients may still have hormonal and neurologic abnormalities caused by the tumor and surgery. This may decrease quality of life. Therefore, it is fundamental for patients to have a robust support system from family and medical professionals.
The first surgery is the best chance at removal of the most amount of the tumor safely. Therefore, choose your surgeon wisely.
In summary, craniopharyngiomas are rare benign tumors that benefit from multidisciplinary team management due to their complexity and associated complications. Surgery is typically the primary treatment option. When it is safe and feasible, the objective of surgery is to achieve complete total tumor resection.
Advances in techniques and equipment have allowed the minimally invasive transnasal approach to be of greater use. A high percentage of patients reach at least 10 years of survival following surgery. A strong support system and medical team are fundamental to optimize treatment outcomes.
Key Takeaways
- Craniopharyngiomas are rare and relatively benign tumors of the central nervous system, and surgery is the primary treatment.
- Among the surgical approaches, the transcranial and transnasal routes are commonly used. The choice is determined by the tumor size, location, and extension.
- A multidisciplinary medical team is an essential aspect of optimal patient management before, during, and after the surgery.
- Patients require long-term socio-economic, neurologic, and endocrinologic support to manage the complications associated with the tumor and the surgery/radiation therapy.