Awake Craniotomy: What the Patient Needs to Know
Overview
Awake craniotomy, also known as awake brain surgery, is a procedure where the patient is awake for a portion of the operation. This is usually performed for brain tumors (mainly low grade gliomas) near critical areas in the brain involved in functions such as speech, movement, or sensation.
Functional areas are mapped by having the patient perform tasks while the brain is painlessly stimulated. If voluntary function is temporarily lost during the stimulation, the area is marked and preserved during tumor removal. Although this may seem like a frightening experience, patients communicate with their surgeon and operating room team to ensure maximal comfort throughout the procedure. The patients are also slightly sedated to be comfortable during the process.
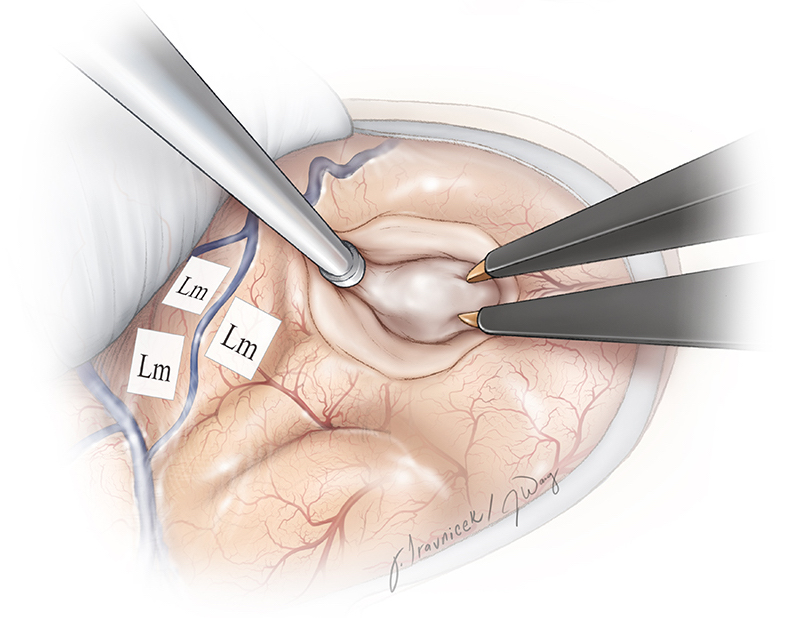
Figure 1. Critical areas are tagged with small paper labels and avoided during tumor removal.
What Is an Awake Craniotomy?
An awake craniotomy, also known as awake brain surgery, is a surgical procedure where a patient is woken up for one part of the operation. The name “awake craniotomy” is slightly misleading, as the patient is heavily sedated when the more painful part of the procedure, in other words, craniotomy (skin incision and bone flap removal) is being performed.
When the surgeon begins operating near areas that are critical for functions such as speech, the patient is awakened (sedation decreased) and he/she helps the surgeon to map which areas of the brain are responsible for these critical functions. This can be done by simply having a conversation with the neurosurgeon and anesthesiologist while the surgery is taking place or performing simple tasks. This is a relatively painless procedure as the brain tissue itself cannot feel pain.
Awake craniotomies may be performed more frequently for cases of low-grade glioma or brain metastases when the tumors are close to nearby structures. This helps to maximize tumor removal while avoiding neurologic complications. However, awake craniotomies are not suitable for everyone. Patients must be able to remain calm and cooperative for 4 – 5 hours.
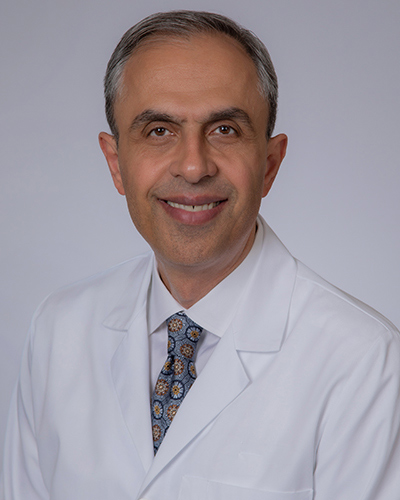
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.

Figure 2. Mapping the face area. The patient must be comfortable. The patient-surgeon interaction is key to success.
Who Performs Awake Craniotomy?
An awake craniotomy is performed by a neurosurgeon who works with an anesthesiologist and neurologist. Speech therapists and neuropsychologists may also be present in the operating room to help observe and make judgments. Oncologists and rehabilitation experts are often involved in the aftercare.
What Happens Before Awake Craniotomy?
Before awake craniotomy, the surgeon will explain what the procedure will entail, its risks and its benefits. Awake craniotomy may seem like a frightening experience but knowing exactly what to expect can significantly help to alleviate anxiety. Other paperwork will be filled out to inform the surgeon of relevant medical history such as allergies, other medications the patient is taking, reactions to anesthesia, and any previous surgeries.
One week before surgery, non-steroidal anti-inflammatory (NSAID) medications such as ibuprofen (e.g. Advil, Motrin), naproxen (e.g. Aleve), and other prescribed NSAIDs, as well as blood thinners such as warfarin (e.g. Jantovin, Coumadin), acetylsalicylic acid (e.g. Aspirin), and clopidogrel (e.g. Plavix) should be stopped to decrease the risk of bleeding. This is not an all-inclusive list. Inform your physician of all medications and supplements you are taking and follow their recommendations.
Several days before surgery, a physical exam, blood tests, electrocardiogram, chest X-rays and other tests may be performed to ensure that your body can safely handle the surgery and that surgical scenarios (e.g. bleeding) are properly prepared for. A baseline neurological exam is conducted and repeated after surgery to check for any neurological changes that may have occurred during the operation. An MRI may be scheduled if the surgeon plans to use image-guidance during the operation.
On the night before the surgery, your physician will ask that you not eat or drink anything (fasting) to prevent vomiting while under sedation. To reduce the possibility of infection at the site of incision, showering or washing your hair with a special antiseptic shampoo may be required.
What Happens During Awake Craniotomy?
Awake craniotomy may take 4 to 6 hours, depending on your underlying condition. We discuss below the steps in an awake craniotomy with language mapping. Similar steps apply for mapping movements in the arms and legs.
Step 1: Patient Preparation
The patient is placed on the operating table and given appropriate anesthesia. Some surgeons prefer the patient to be relatively awake throughout the entire procedure, while others prefer that the patient is awake only during the mapping and tumor removal stages.
After the patient is heavily sedated, a three-pin skull clamp is connected to the table and the patient’s head to immobilize the head during the procedure. Local anesthetic is used to place the pins on the head. Pillows and other comfort measures will be provided to ensure that the neck is comfortable and pressure points are padded.
Warming blankets may be used to minimize shivering. If the patient is awake at this time, communication with the surgeon is important to ensure that the patient’s position is comfortable and can be easily tolerated for the next few hours.
When the position is set, the patient’s hair is shaved or clipped in the area of the incision/craniotomy. Alternatively, a hair sparing technique may be used. This technique shaves only a ¼-inch wide area around the planned incision line. A line is drawn on the scalp to mark the path of the initial incision.
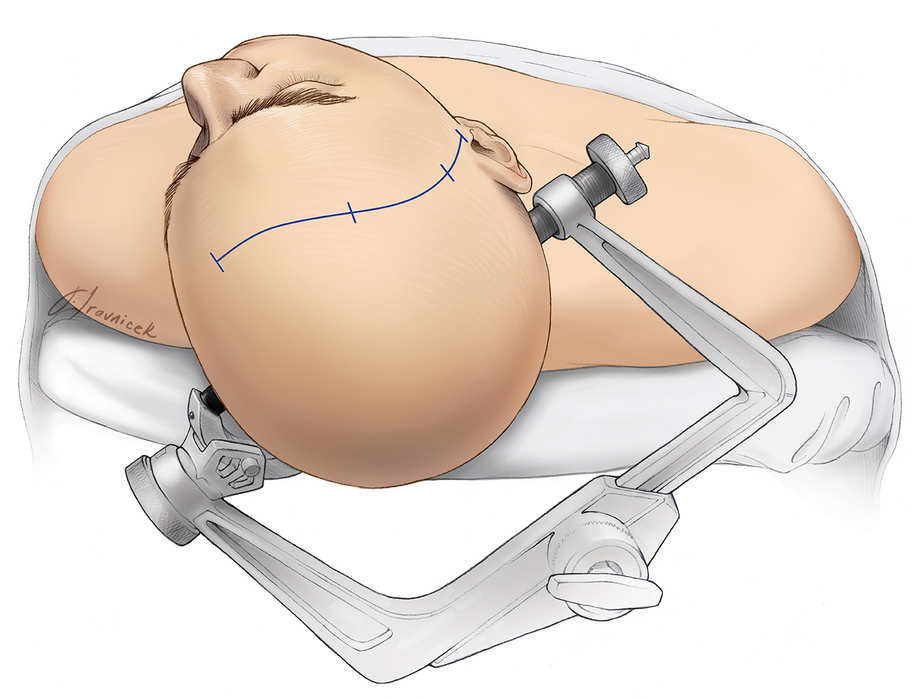
Figure 3. While under sedation, the patient’s head is positioned and immobilized via a three-pin skull clamp.
Step 2: Skin Incision
The skin around the incision line is scrubbed with an antiseptic to reduce the possibility of infection. A skin incision is made through the scalp to the outer surface of the bone. Clips are applied to the edges of the scalp to minimize bleeding.
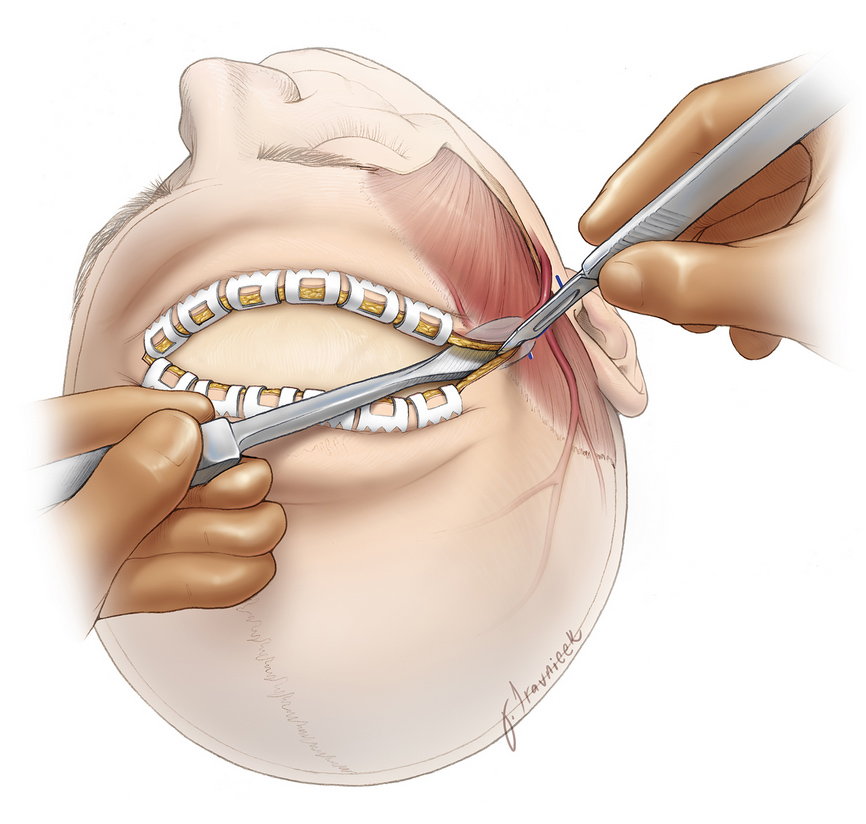
Figure 4. The scalp is cut and then clips are placed on its edges to minimize bleeding.
Step 3: Craniotomy
Muscles, if present, are flapped back and secured. A small opening in the skull (burr hole) is made with a surgical drill called a perforator. A blunt-ended tool is inserted into the burr hole and used to separate the outer covering of the brain (dura) away from the inner aspect of the skull bone. Another instrument called the craniotome is then used to saw through the bone from the initial burr hole to create a removable bone flap.
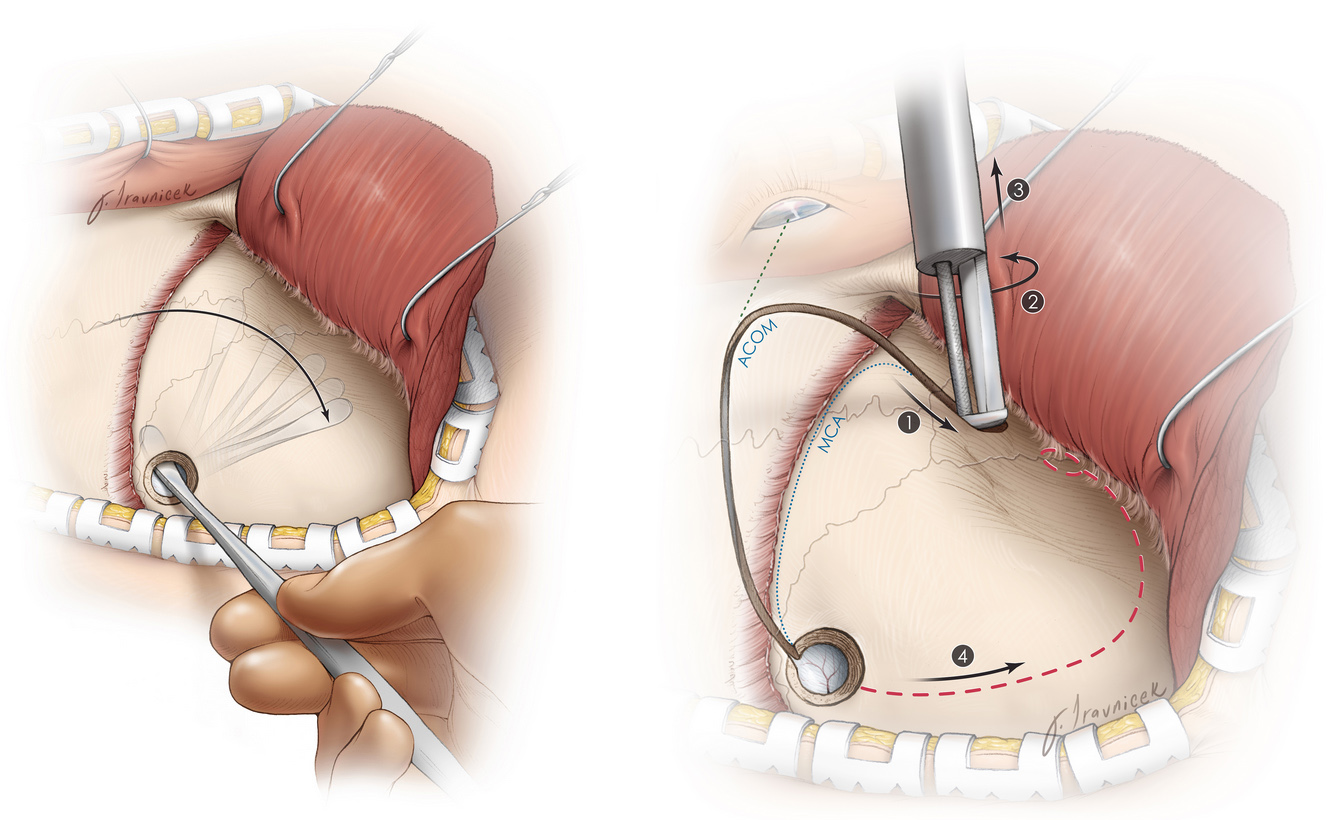
Figure 5. A blunt dissector is placed through the burr hole and swept under the bone to separate the dura from the bone (left). A craniotome with a footplate is used to saw through the bone and create the bone flap (right).
Step 4: Brain Exposure and Surgery
The dura is cut open and flapped back. It may be temporarily secured to the muscle with sutures. The surgeon can then use a variety of tools such as scissors, dissectors, ultrasonic aspirators and more to operate on the brain and treat the underlying condition (e.g. removal of a brain tumor).

Figure 6. The dura is cut and reflected back.
Step 5: Awake Mapping
When the tumor is reached, sedative medications are stopped to allow the patient to awaken and prepare for the mapping procedure. Electrical stimulation is applied to an area of the brain for 2 – 3 seconds (remember, this is not painful). The patient is presented with a task such as naming a picture or counting from 1 to 20, and the accuracy of their response is recorded.
Each site is checked three to four times, so the patient may have to answer many simple questions. If stimulation at a site causes language dysfunction such as loss of speech, the area is labeled with a small tag that tells the surgeon to preserve this area during tumor removal.
Loss of voluntary function may produce anxiety and fear. However, this is only temporary during the stimulation procedure and used to preserve neurologic function. Once tumor resection begins, language exams are continuously performed to ensure that neurologic function remains intact. If any slight deficit occurs, the surgeon stops further resection.

Figure 7. Tumor removal is guided based on the mapping data.
Step 6: Closure
After the operation within the brain is complete, the patient is more sedated for the rest of the procedure. The dura is then sutured back together, and the bone flap is reattached using small titanium plates and screws. These remain there permanently and may sometimes be felt under the skin. Muscles and connective tissues are reaffixed to their original position. Finally, clips are taken off of the scalp and the edges are sutured.
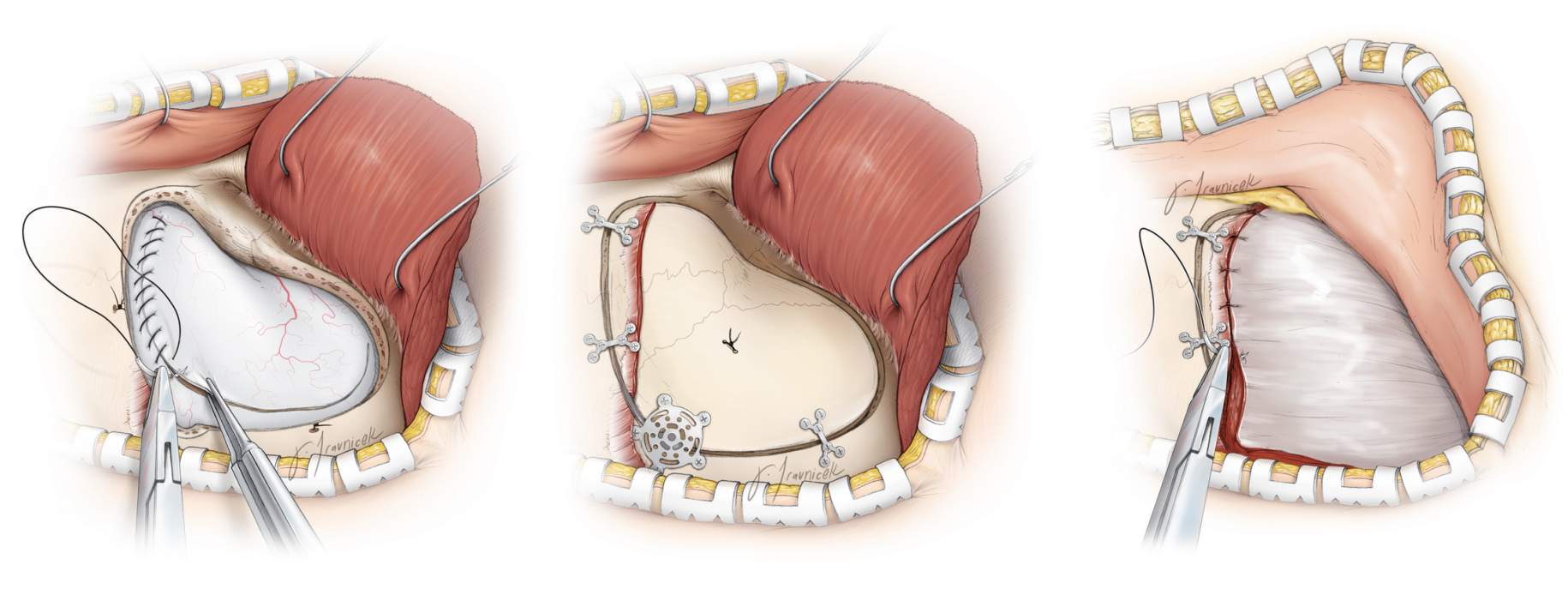
Figure 8. The dura (left), bone flap (middle), and muscle and connective tissues (right) are reattached with sutures for tissue and metal plates for bone.
What Happens After Awake Craniotomy?
Immediately after completion of an awake craniotomy, you are taken to a recovery room for monitoring as the anesthesia wears off. Once you are fully awake, you are taken to the intensive care unit (ICU) for further monitoring and control of blood and intracranial pressures, nutrition, temperature, oxygen levels, pain, and more.
Antibiotics and antiseizure drugs are typically administered. Imaging is often performed within 48 hours to ensure that the tumor was maximally removed. A neurologic exam is conducted to check for signs of early complications such as impaired consciousness, seizure, strokes, or intracranial bleeding.
Most patients experience pain after brain surgery. This is controlled with medications such as narcotics (e.g. morphine, fentanyl, or hydromorphone), acetaminophen (Tylenol), muscle relaxants (e.g. methocarbamol, diazepam, tizanidine), or steroids (e.g. dexamethasone).
High blood pressure, nausea and vomiting, and shivering may occur and can be addressed with medications and blankets or air warming devices. Temporary neurologic deficits may occur after the procedure but these should most often resolve during the recovery period.
After a few days or once your condition has stabilized, you are transferred to the regular hospital ward. Getting out of bed and walking as tolerated is encouraged and a physical therapist may be asked to work with you. Depending on the complexity of the operation, the total hospital stay may range from a few days to 1-2 weeks. Inpatient rehabilitation may be necessary to allow for efficient recovery of temporary neurological deficits.
At home, you should follow the instructions provided by your surgeon. A follow-up appointment may be made in the next 1 – 2 weeks. During recovery, you may have issues with walking, talking, strength, and balance. Headaches that are described as pulsating or pounding are common and can persist for several months after surgery. In general, avoid high-intensity activities, keep the incision site clean, and take pain medicine as directed. Discuss when you can return to work with your surgeon. You may not be able to return to work for several weeks.
Activities
- Avoid strenuous activity (e.g. lifting heavy items, jogging, sex)
- Avoid risky activities that require your attention (e.g. driving)
- Do not drink alcohol or use nicotine products (e.g. smoking, vaping)
- Try to walk 5 – 10 minutes daily, and gradually increase this as you recover
- Sleep with your head elevated and apply ice 3 times a day for 15 minutes to reduce pain and swelling
- Drink water and eat foods high in fiber (e.g. beans, whole grains, nuts, berries) to resolve constipation caused by the narcotics used for pain control during or after surgery
- Discuss activities such returning to work or air travel with your surgeon
Incision Care
- Shower as early as two days after surgery
- Gently wash the incision site with soap and water daily
- Avoid hair styling products, lotions, baths
Medications
- Take acetaminophen (Tylenol) for headaches and other pain medications as directed by your physician
- Do not take NSAIDs (e.g. Advil, Aleve), blood thinners (e.g. Aspirin, Coumadin) or other supplements without surgeon’s approval
When to Call Your Doctor
- Fever or chills
- Redness, swelling, bleeding, increased pain around the incision site
- Swelling at the incision site with clear fluid leaking from your ears or nose
- Excessive sleepiness, confusion, increased headaches, weakness in your arms or legs
- Vision, speech, or breathing problems
- Green, yellow, or blood-tinged sputum (phlegm)
- Seizures
What Are the Possible Complications?
The most common side effect of intraoperative stimulation are seizures, though serious injury due to seizures has not been reported. Other possible complications of awake craniotomy include reactions to sedation such as nausea and vomiting, pain at the craniotomy site, swelling and bruising of the face, infection, bleeding, stroke, seizures, brain swelling, and cerebrospinal fluid leak.
A dent may be present where the bone flap was removed. If the craniotomy is performed near the temples, the temporalis muscle may be cut. This muscle helps with chewing. After the operation, the muscle on the side of the craniotomy may be slightly shortened and cause a feeling of jaw stiffness. This problem usually resolves within a few months.
Rarely, a blood clot forms near the site of the craniotomy. If large, this may be removed with another operation.
What Is the Recovery Outlook?
After awake craniotomy, the bone flap will mend itself over time and partially heal back into the rest of the skull bone within 2 to 3 months. Full recovery may take a few months and depends on the underlying condition being treated. Although the thought of being awake during brain surgery can seem frightening, most patients report overall satisfaction with the procedure. Communication with the surgeon and operating room team is important to alleviate anxiety and remain comfortable during the operation.
Temporary neurological deficits are not uncommon, but most patients will recover almost completely within 1-3 months after surgery.
Glossary
Bone flap—section of bone temporarily removed during a craniotomy
Burr hole—small opening through the skull made by a surgical drill
Cerebrospinal fluid—clear fluid that surrounds the brain and spinal cord
Craniotome—special neurosurgical saw that enables a surgeon to cut through the bone without cutting the dura mater
Craniotomy—procedure that removes a piece of bone from the skull to expose the brain; the bone is reattached to its original location immediately after the rest of the surgery
Dura mater—outermost covering of the brain
Seizure—sudden burst of abnormal electrical activity in the brain that leads to uncontrollable spasms, twitching, or jerking
Contributor: Gina Watanabe BS
References
-
Szelényi A, Bello L, Duffau H, et al. Intraoperative electrical stimulation in awake craniotomy: methodological aspects of current practice. Neurosurgical Focus. 2010;28(2):E7. doi:10.3171/2009.12.FOCUS09237
-
Milian M, Tatagiba M, Feigl GC. Patient response to awake craniotomy – a summary overview. Acta Neurochir. 2014;156(6):1063-1070. doi:10.1007/s00701-014-2038-4