Meningioma Subtypes and Locations

A diagnosis of a meningioma can be difficult for both patients and caregivers. Here, we will try to answer common questions you may have about your diagnosis. Please remember to discuss any additional questions or concerns you may have with your care team.
What Are the Different Types of Meningioma?
A meningioma is a type of tumor that originates from the meninges, which is a protective covering of the brain and spinal cord. While meninges are not part of the brain itself, a meningioma can cause symptoms such as headache, confusion, drowsiness, nausea, vomiting, changes in vision, or seizures because the meningioma may disrupt the functions of the brain by pushing on or compressing important structures in the nervous system.
The types of meningioma symptoms you or your loved one may be experiencing can help explain where a meningioma might be located. Meningiomas are slow-growing and often compress different parts of the brain. Pressure on different parts of the central nervous system causes different symptoms.
In fact, meningiomas can be classified based on where they are located. The meningioma location will help your care team design treatment decisions including developing a plan for surgery, if needed. Occasionally, meningiomas may be in an area that is difficult to safely remove surgically. In these cases, alternative treatment options may be used.
Below is a list and description of some of the most common locations for meningiomas. This is not a complete list, and we would encourage you to discuss with your care team what the location of you or your loved one’s meningioma means for treatment.
Parasagittal meningioma: The brain is separated into a left and right side by a divider (falx cerebri) that is made up of meninges. Parasagittal meningiomas grow on this divider between both sides of your brain.
Cerebral convexity meningioma: These meningiomas grow off the protective covering along the top of your brain.
Suprasellar meningioma: These meningiomas are located near the front of your brain and just behind your eyes and the bridge of your nose. Since this tumor is near where your eyes communicate with your brain, some patients may experience changes in vision.
Sphenoidal ridge: These meningiomas grow on the lining near the base/bottom of your brain. An exterior landmark for this location would be in the space between your ear and eye.
Olfactory groove: Olfaction is another name for your sense of smell. These meningiomas develop where your nose nerves connect to your brain. As a result, patients may experience a loss of smell. These tumors can affect personality due to their vicinity to the base of the frontal lobes and can reach a giant size.
Clivus meningioma: These meningiomas grow off of the protective covering at the bottom of the brain or along the skull base, near the brain stem, which is where the brain communicates with the rest of the body.
Foramen magnum meningioma: The foramen magnum is a hole at the bottom of the skull that allows your brain to connect to the rest of your body through your spinal cord. You may feel the back part of this hole by pressing on the back of your neck where it meets with the bone of your skull.
Cerebellar meningioma: These meningiomas are typically located on the protective covering of the cerebellum. People with meningiomas in this area may experience a loss of balance, vertigo, and nausea. This is because the meningioma may put pressure on the cerebellum which is the part of your brain that controls balance.
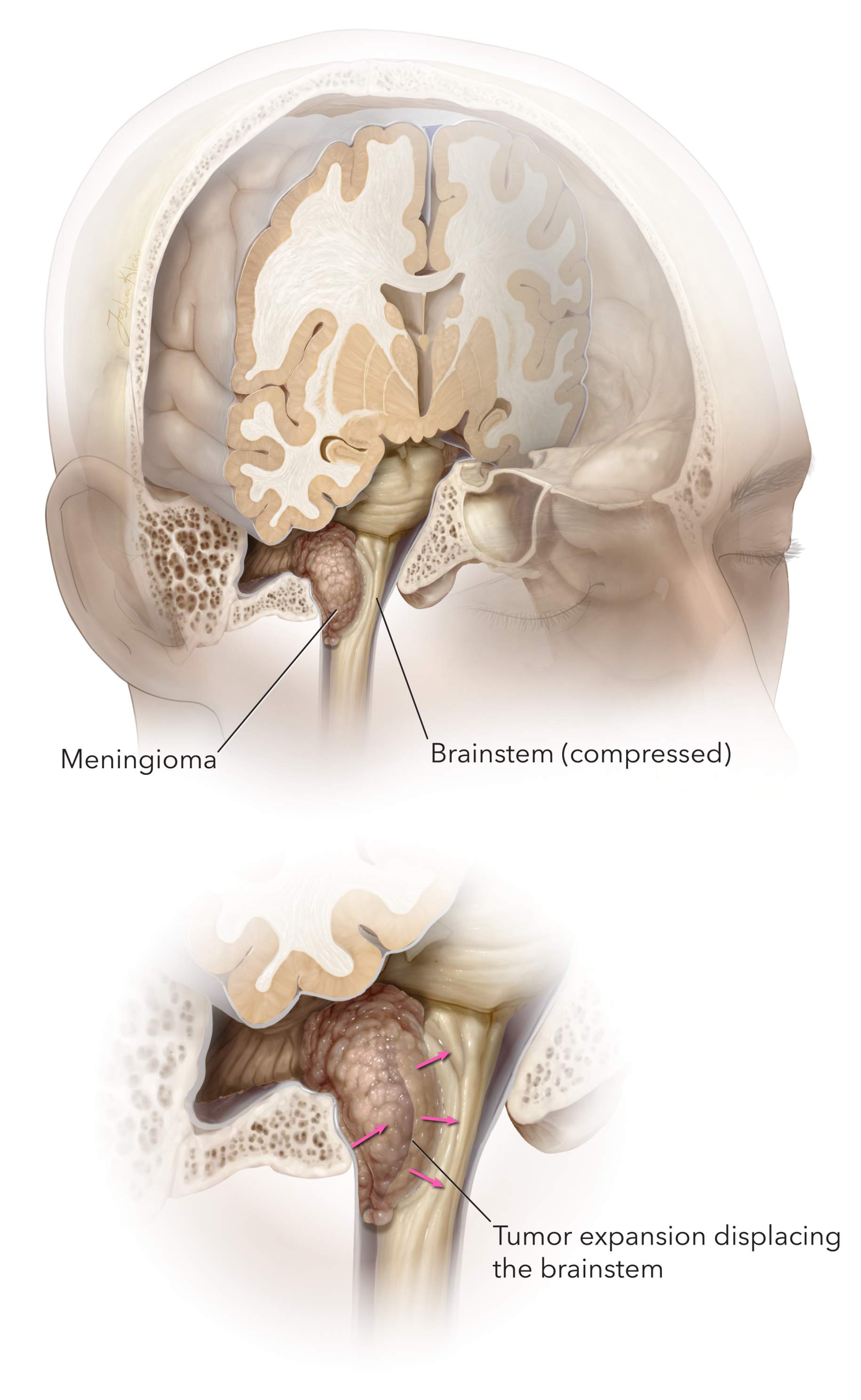
Figure 1. Meningiomas can compress any part of the brain including the brainstem and lead to numerous symptoms.
Posterior Fossa/Petrous Meningioma: A posterior fossa meningioma is a non-cancerous growth occurring in the skull's rear section near the brainstem and cerebellum. On the other hand, a petrous meningioma is specifically located in the petrous bone that forms the skull's base. These tumors may cause headaches, hearing loss and balance issues.
Sphenoid Wing Meningioma: This particular type originates from the sphenoid bone, which forms the central base of the skull and is also part of the eye socket. Due to their proximity to crucial structures within the brain and eye, sphenoid wing meningiomas can cause vision impairment, facial numbness or headaches.
Intraventricular Meningioma: This type of tumor develops within the brain's ventricular system, the interconnected cavities responsible for the production and flow of cerebrospinal fluid. Intraventricular meningioma can disrupt cerebrospinal fluid circulation, leading to increased pressure within the brain and associated symptoms such as headache, nausea, and cognitive disturbances.
Spinal Meningioma: This type of tumor occurs in the spinal canal, specifically arising from the protective layers surrounding the spinal cord called meninges. It can compress nearby nerves or the spinal cord, causing symptoms such as pain, weakness, numbness or loss of bladder and bowel control.
Intraorbital Meningioma: An intraorbital meningioma is a type of tumor that originates from the tissues surrounding the eye and develops within the eye socket. This condition can lead to vision-related problems, such as eye bulging, eye movement issues and impaired vision.
Planum Sphenoidale Meningiomas: These tumors develop in the region of the skull known as the planum sphenoidale. This region forms the roof of the sinus cavity and is located under the brain's frontal lobe. Due to their proximity to important structures such as the optic nerves and pituitary gland, planum sphenoidale meningiomas can cause headaches, visual disturbances and hormonal imbalances.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
What Is the Average Size of Meningiomas?
Meningiomas may be discovered in one of two ways. In the first, they may be found on a brain scan that was obtained for another reason. These tumors are considered incidental. In the second, patients may develop relevant symptoms that lead to a scan of their head resulting in the discovery of a meningioma.
Since the cause of symptoms from a meningioma are due to pushing or compressing of the brain, symptomatic meningiomas tend to be larger with an average diameter of 4.6 centimeters (approximately the size of a golf ball).
Alternatively, incidentally discovered meningiomas have an average diameter of 2.3 centimeters (approximately the size of a gumball). Smaller, incidentally discovered meningiomas are often observed with serial imaging (every 6-12 months) and may not require treatment unless they significantly grow.
It is important to emphasize that not every meningioma needs treatment. Therefore, you should not stress about living with a small benign meningioma. Surgery for its removal may pose more risks to you than leaving it alone.
What Size Meningioma Is Considered Large? What Size Is Considered a Small Meningioma?
The size of meningiomas may be considered large if they are greater than 3 centimeters in diameter or giant if they are larger than 5 centimeters in diameter. Larger meningiomas may be more difficult to treat surgically in terms of their complete removal, depending on where they are located.
Although most large and giant meningiomas require surgical treatment, the decision for removal of smaller meningiomas (less than 3 centimeters in diameter) must be individualized.
At What Size Does a Meningioma Need To Be Removed?
The need to remove a meningioma typically depends on its location, symptoms and growth rate rather than on a specific size. However, meningiomas larger than three centimeters often require surgical intervention. The reason for this is that the tumor is already causing significant symptoms when it reaches this size. Still, a neurosurgeon will evaluate the specific case to determine if and when a meningioma needs to be operated.
Can a Meningioma Be Fatal?
The pathological grade given to all meningioma subtypes can be used to determine the outcome of tumor regrowth/prognosis and guide treatment decisions.
Grade I meningiomas are considered benign, are less likely to recur following treatment and are rarely fatal. Grade II and III meningiomas are more challenging to treat and can be fatal due to their higher chance of recurrence.
You may hear you or your loved one’s care team discussing a 5-year relative survival rate. For grade II and grade III meningiomas, the relative survival rate is 63.8%. This relative survival rate means that someone with a grade II or III meningioma is about 63.8% as likely as people without this tumor to live for at least 5 more years.
While this relative survival rate may be helpful, it does not account for the individual factors such as age, response to treatment, or traits of the tumor itself that influence you or your loved one’s outcome. It is important to discuss your individual case with your care team to have a better understanding of long-term outcomes.
Understanding Your Care
Receiving a diagnosis of meningioma presents a difficult challenge. The treatment and outcomes following diagnosis of a meningioma are individualized to you or your loved one’s specific circumstances.
It is important to remain informed by asking your care team questions and clarifying anything you are uncertain of. Remaining informed can help you be an active participant in decisions regarding your care.











