Surgery for Dural Arteriovenous Fistula


Dural arteriovenous fistulas (dAVFs) represent abnormal connections between arteries and veins located within the dura mater, the outermost layer of the protective coverings of the brian and spinal cord.
These rare vascular abnormalities can present with a range of symptoms, including vision changes, speech difficulties, tinnitus (rhythmic ringing or whooshing in the ears), cognitive changes, seizures, weakness, and loss of bowel or bladder control.
The precise cause of dAVFs often remains elusive. However, certain factors have been associated with an increased risk, such as prior surgical procedures and hereditary blood vessel or blood clotting disorders.
Diagnosing dAVFs typically involves advanced imaging techniques like computed tomography (CT), magnetic resonance imaging (MRI), and angiography. These methods help visualize the abnormal blood flow patterns, dilated blood vessels, and signs of venous congestion or bleeding near the dura.
Options for treatment can range from observation for asymptomatic cases to more active interventions like embolization, where catheters are used to block abnormal connections, or surgical procedures to repair or reroute blood flow.
The choice of treatment is individualized, considering the specific characteristics of the dAVF and the patient's overall health, and is typically determined in consultation with a medical specialist. In this article, we will take a look surgery to treat dAVFs and will attempt to answer questions you or a loved one may have.
Can Surgery Treat or Fix dAVFs?
When endovascular embolization proves unsuccessful or is deemed impractical, surgical resection becomes a viable option for treating dural arteriovenous fistulas (dAVFs).
Surgical treatment for dural arteriovenous fistulas (DAVFs) involves carefully closing off the abnormal connections between the arteries and veins in the dura mater, which is the tough outer layer that covers the brain and spinal cord. Here's a simplified description of the process:
- Preparation: Before surgery, doctors use imaging tests like angiography to see the blood vessels and find the exact location of the DAVF.
- Anesthesia: The patient is put to sleep with general anesthesia to ensure they are comfortable and do not feel pain during the procedure.
- Incision: The neurosurgeon makes an incision in the scalp and creates a small opening in the skull, called a craniotomy, to access the affected area of the dura mater.
- Microsurgical Disconnection: Using a microscope to see the small vessels, the surgeon carefully separates the abnormal connections between the arteries and veins. This might involve cutting and sealing the vessels or using tiny clips to close them off.
- Closure: Once the fistula is disconnected, the surgeon replaces the bone and closes the incision in the scalp.
- Recovery: After surgery, the patient is monitored closely in the hospital. They may need follow-up imaging tests to make sure the DAVF is completely treated.
Angiography may be employed during the operation to precisely identify the affected blood vessels. This real-time imaging technique aids in ensuring complete obliteration of the fistula, enhancing the overall success of the surgery.
This procedure aims to restore normal blood flow and reduce the risk of further complications, such as intracranial hemorrhage.
The decision to pursue surgery for dAVFs is typically based on factors such as the type, location, and severity of the fistula, as well as the patient's overall health. It is important for the approach to be individualized, with thorough consideration given to the specific characteristics of the dAVF, and the treatment plan is usually determined in consultation with skilled and well-trained neurosurgeon.
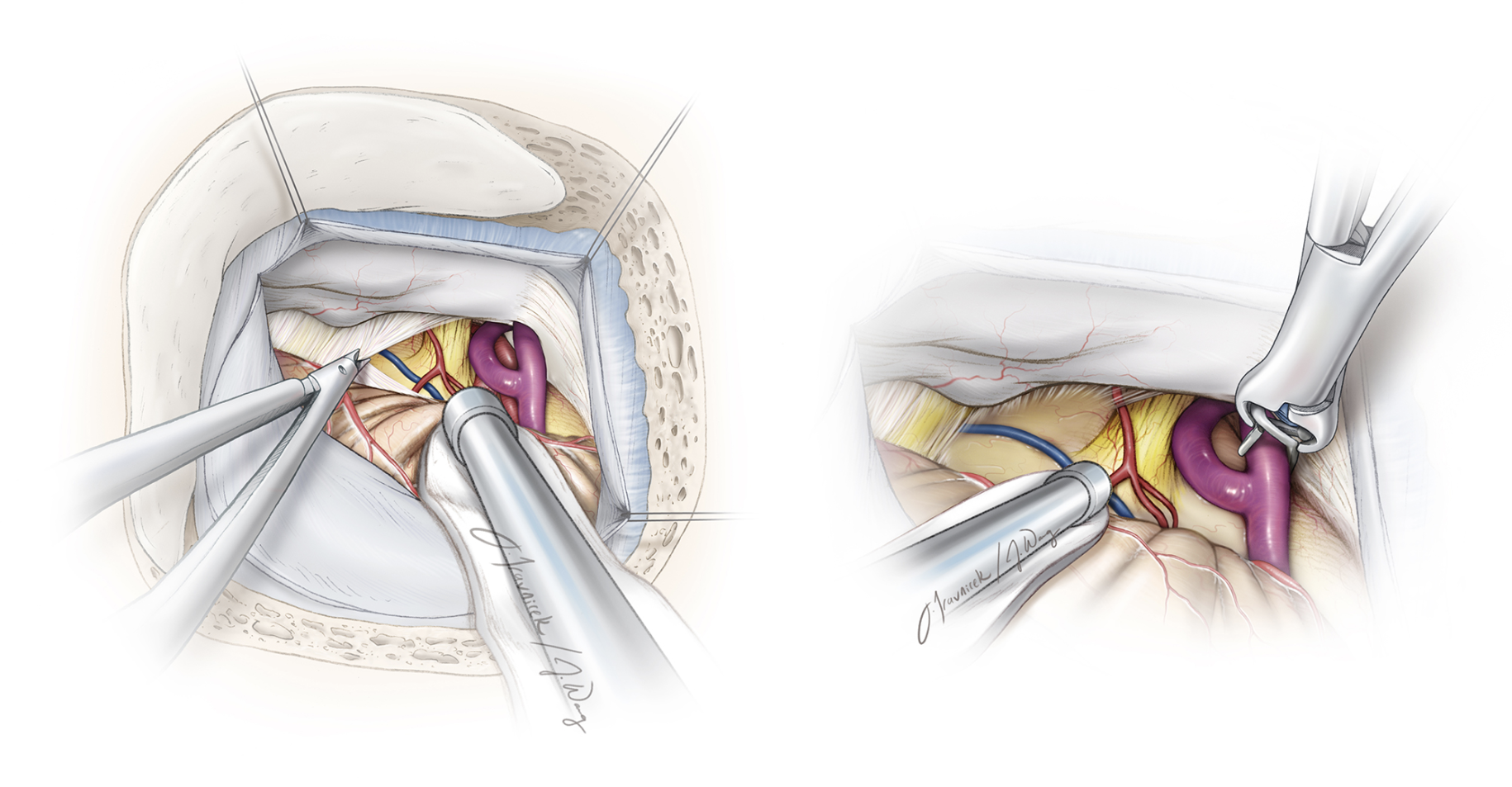
Figure 1: Illustration of microsurgical clipping of a skull base dAVF.
What Are the Most Common Complications?
The most common complications associated with dural arteriovenous fistula (dAVF) treatment include postoperative hemorrhage, neurological deficits, and infection. Postoperative bleeding can occur due to the intricate nature of dAVFs, involving abnormal connections between arteries and veins, and the manipulation of delicate tissues during surgery.
Neurological deficits may arise from inadvertent damage to surrounding structures during the intervention. Infection is a potential complication and can occur at the surgical site.
Additional surgical complications can also include the accumulation of excess fluid within the ventricles (brain cavities), known as hydrocephalus, as well as the occurrence of cerebrospinal fluid leaks, strokes, and even death.
As seen by these serious complications, this is considered a major surgery and seeking an experienced neurosurgeon is essential.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
How Long Does Arteriovenous Fistula Surgery Take?
The duration of arteriovenous fistula (AVF) surgery can vary depending on factors such as the complexity of the fistula, its location, and the chosen surgical approach. In general, AVF surgeries may take several hours to complete. The procedure involves careful dissection, identification, and repair of the abnormal vascular connections between arteries and veins.
Is dAVF Surgery Urgent?
The urgency of fistula surgery depends on several factors, including the specific type and severity of the fistula, as well as the symptoms it presents. In some cases, surgery for a fistula may be considered urgent.
Urgency is determined when the lesion poses an immediate threat to the patient's health or if there is an imminent risk of acute disease-related complications such as bleeding or neurological deficits.
However, for asymptomatic or less severe cases, surgery may be less urgent, and more time may be given. The decision on the urgency of fistula surgery is typically made through a collaborative effort involving the healthcare team.
Every member of the care team is active in considering the individual patient's condition and the potential risks associated with delaying the intervention.
Other Treatment Options for Arteriovenous Fistula
In addition to open surgical and endovascular treatments, there are other options for dural arteriovenous fistulas (dAVFs) depending on the specific characteristics and severity of the condition.
Radiosurgery is another non-invasive option that employs highly focused radiation beams to target and close off the dAVF, over time. Radiosurgery carries its own risks, benefits, and side effects, and they are discussed in more depth, here.
Observation, or "watchful waiting," of a dAVF may be considered in cases that are not presently exhibiting symptoms, or risk factors for an individual patient may be prohibitive.
Key Takeaways
- A dural arteriovenous fistula (dAVF) is an unusual connection between blood vessels in the brain and spinal cord's outer covering. It can cause symptoms like vision issues, seizures, ringing in the ears, weakness, or bowel and bladder problems.
- Doctors use imaging tests like CT, MRI, and angiography to see these unusual blood vessel connections clearly.
- If a dAVF isn’t causing symptoms, doctors might just monitor it. For active treatment, options include minimally invasive procedures to block the abnormal vessels or surgery for more complex cases.
- Surgery to remove abnormal vessels may be considered when other treatments don’t work. Surgeons use real-time imaging to help guide the procedure safely.
- The urgency of surgery depends on the dAVF’s location and symptoms. Non-surgical options like radiosurgery may also be available for smaller dAVFs.











