Symptoms of Arteriovenous Fistulas

An arteriovenous fistula (AVF) is an abnormal connection between an artery and a vein, found in the circulatory system. When a fistula develops in proximity to the outer brain covering, known as the dura, it is referred to as a dural arteriovenous fistula (dAVF).
Normally, arteries carry oxygen-rich blood away from the heart to supply tissues and organs, while veins return oxygen-depleted blood back to the heart. In the case of an AVF, an artery and a vein are directly connected without the usual capillaries in between, disrupting the natural flow of blood.
This condition can occur due to various reasons, such as trauma, congenital malformations, or because of certain medical procedures like dialysis access creation.
Dural AVFs are of particular significance because they can cause several health issues. The symptoms associated with dAVF encompass headaches, nausea, vomiting, seizures, speech or language difficulties, dementia, instability, visual deterioration, and protrusion of the eyes.
Moreover, untreated or poorly managed AVFs can lead to problems like swelling, pain, high-output heart failure, and a risk of clot formation, which may necessitate medical intervention or surgical repair to restore normal blood circulation. In this article we will take a deeper look into the symptoms associated with AVFs and try to answer any questions you may have.
What Are the Symptoms of an Arteriovenous Fistula?
The symptoms of an arteriovenous fistula (AVF) can vary depending on its location and size. For intracranial dural arteriovenous fistulas (dAVFs), symptoms often relate to the location of the fistula and the pattern of venous drainage. Common symptoms include:
- Pulsatile Tinnitus: A whooshing sound in the ear that matches the rhythm of your heartbeat.
- Headache: Often feels like a constant, localized pain.
- Neurological Deficits: This can include weakness, numbness, or other specific problems related to nerve function.
- Visual Disturbances: This might involve vision loss, redness in the eyes, bulging eyes, or double vision, especially with certain types of blood vessel issues in the brain.
- Intracranial Hemorrhage: Sudden symptoms like a severe headache, nausea, vomiting, changes in consciousness, or problems with movement or sensation.
- Seizures: These can occur due to irritation in the brain caused by blood flow issues or bleeding.
- Myelopathy: In cases of spinal blood vessel problems, symptoms may include back pain, weakness, changes in sensation, or trouble with bladder and bowel control.
For peripheral AVFs, symptoms might include swelling, a palpable thrill or audible bruit over the site of the fistula, and potential ischemia distal to the fistula due to a "steal" phenomenon.
It's important to note that some AVFs can be asymptomatic and discovered incidentally during imaging for other reasons. Diagnosis and management should be tailored to the individual patient, considering the location and hemodynamic impact of the AVF.
What Are the Causes of dAVFs
Arteriovenous fistulas (AVFs) can develop for various reasons, including congenital factors, trauma, or medical procedures. Congenital AVFs occur due to abnormal vascular development during fetal growth, leading to a direct connection between arteries and veins.
Traumatic AVFs can result from injuries, such as penetrating wounds or blunt force trauma, that damage blood vessels and cause them to form abnormal connections. Additionally, certain medical procedures, like catheterization or surgical interventions, can inadvertently create AVFs if there is unintended damage to nearby blood vessels during the process.
It is worth noting that while these examples illustrate our best understanding of the process of AVF formation, the underlying mechanism is still unknown.
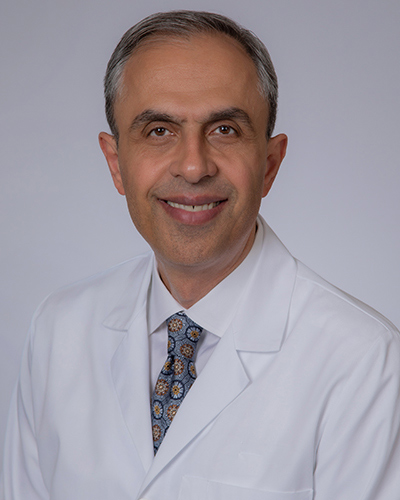
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
How Are dAVFs Diagnosed?
Dural AVFs are typically first diagnosed through imaging techniques such as computed tomography (CT) or magnetic resonance imaging (MRI). These imaging methods can reveal dilated blood vessels with venous congestion, indications of elevated blood pressure, or signs of bleeding.
When abnormal blood flow patterns near the dura are detected, angiography is often employed for a more detailed examination. Angiography is a minimally invasive procedure that involves the insertion of a catheter into an artery, guiding it through blood vessels to the brain, and injecting contrast dye near the targeted blood vessels.
Once the contrast has been injected, subsequent X-ray images and videos are taken. These high-resolution images very clearly capture the vascular structure and the flow of blood from arteries to veins, aiding in the diagnosis and assessment of dAVFs.
How Are dAVFs Treated?
The treatment of dural arteriovenous fistulas (dAVFs) depends on various factors, including the type, location, and severity of the dAVF, as well as the patient's overall health. In some cases, small, asymptomatic dAVFs may be managed through observation alone, where healthcare professionals monitor the condition regularly to ensure it doesn't worsen over time.
However, if the dAVF is causing symptoms or poses a risk of complications, more active interventions may be necessary. Embolization is a common minimally invasive procedure used to treat dAVFs.
During embolization, a catheter is inserted into the blood vessels, guided to the site of the dAVF, and then embolic agents, such as coils or glue-like substances, are injected to block the abnormal connection between the artery and vein. This effectively redirects blood flow through the normal pathways and can help alleviate symptoms and reduce the risk of complications.
In more complex or severe cases, surgical intervention may be required to repair the dAVF, either by closing the abnormal connection or rerouting blood flow. In certain situations, radiosurgery may be considered as an alternative to traditional surgery.
Radiosurgery uses highly focused radiation beams to target and close off the dAVF over time, without the need for incisions or catheterization. The choice of treatment depends on the specific characteristics of the dAVF and the patient's individual circumstances, and it should be determined in consultation with a medical specialist.
Key Takeaways
- Dural arteriovenous fistulas (dAVFs) are abnormal connections between arteries and veins, bypassing capillaries. Dural arteriovenous fistulas (dAVFs) occur near the brain’s outer covering and can cause significant health issues.
- Symptoms vary by location and size, including pulsatile tinnitus, headaches, neurological deficits, visual disturbances, seizures, and, in severe cases, subarachnoid hemorrhage.
- Dural AVFs can be congenital, caused by trauma, or result from medical procedures. Congenital AVFs arise from abnormal fetal vascular development, while traumatic dAVFs may stem from injuries or surgical complications.
- Imaging techniques like CT and MRI reveal dAVFs, and angiography provides detailed vascular mapping for precise diagnosis and treatment planning.
- Treatments depend on dAVF severity and location. Options include monitoring, embolization (minimally invasive), surgical repair, and radiosurgery for complex cases, with the approach tailored to patient needs.