Ependymoma
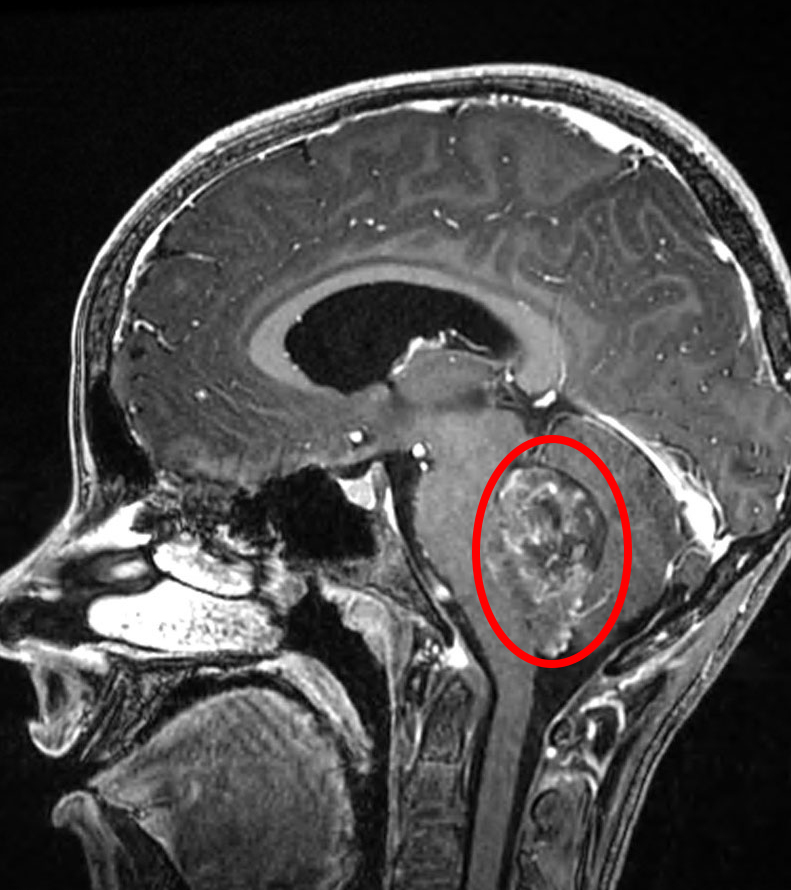
Figure 1: A sagittal MRI demonstrates an ependymoma in the fourth ventricle.
What Is Ependymoma?
Ependymomas are tumors of the central nervous system (brain and spinal cord) made up of ependymal cells. These cells line the cavities of the brain and spinal cord, where they produce cerebrospinal fluid (CSF). Cerebrospinal fluid functions as a cushion for the brain and spinal cord, and provides nourishment for these structures. In children, ependymomas usually grow in the brain. In adults, these tumors usually form in the spinal cord.
What Causes Ependymoma?
Like many tumors, ependymomas are caused by genetic mutations that allow cells to grow and divide uncontrollably. Rare genetic disorders, such as neurofibromatosis type 2, may place patients at an increased risk for developing this type of tumor. Clusters of ependymomas tend to be seen in families, so some genetic factors are thought to be at work.
How Is Ependymoma Diagnosed?
Signs and symptoms of ependymomas are very similar to other tumor types and are largely dictated by the area of the brain that is affected. These signs and symptoms include:
- Headache or back pain
- Nausea and vomiting
- Difficulty walking or maintaining balance
- Seizures
- Double vision or blurred vision
- Problems with eye movement
- Vertigo
Medical history should take into account all of the above signs and symptoms, including how frequent they are, how bad they are (for example, does the pain wake you up at night?) and how long they have troubled you. Next, a physical exam with a focus on neurological changes can pinpoint the likely location of any potential tumor.
When a brain tumor is suspected from the history and physical examination, certain imaging tests may be ordered:
- A computerized tomography (CT) scan is a series of x-rays from different points of view. They are then combined to make two dimensional pictures of the brain with many slices that can be reviewed to give insight into the depth and volume of certain structures.
- Magnetic resonance imaging (MRI) uses magnetic fields, rather than x-rays, to create a similar picture. MRI imaging is the imaging test of choice for ependymomas. Dye contrast is often used to search for metastatic pieces of tumor that may have traveled within the CSF and away from the original tumor location. These metastatic pieces of tumor are often referred to as “drop mets” within the spine.
Why should you have your surgery with Dr. Cohen?
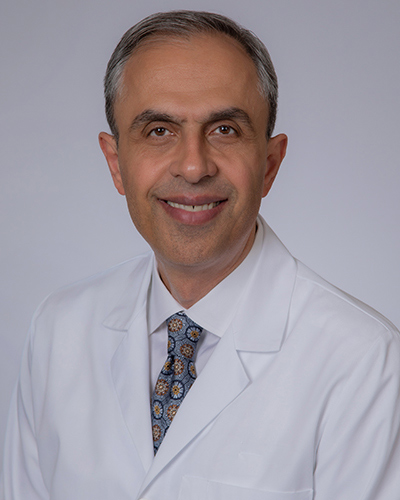
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
How Is Ependymoma Treated?
Once a diagnosis is made via imaging or potentially a biopsy, treatments can be discussed:
- Surgery through a craniotomy is the first line of therapy to remove ependymomas within the brain. Maximal resection (removing as much of the tumor as possible without damaging other brain structures nearby) is the primary goal when removing ependymomas.
- Spinal cord ependymomas can be removed through a small incision in the neck or back. Usually there is little disruption of the vertebrae, which are the individual bones that make up your spine.
- After removal of the tumor and confirmation of an ependymoma, a lumbar puncture, or spinal tap, may be performed to check for the presence of tumor cells in the CSF around other locations of the brain and spinal cord. A small caliber needle is inserted in the lower back and CSF is removed for analysis in the pathology lab. The pathologist will look for any tumor cells.
- Ependymomas are sensitive to radiation therapy. Radiation therapy is more commonly used for ependymomas within the brain than those within the spine. In patients under 3 years of age, radiation therapy is generally avoided and reserved for recurrent cases when other treatments have failed.
- Chemotherapy has not yet proven to be particularly effective; however, drug trials may be available. These trials often do not require insurance, and some even pay patients for their time.
What Is the Prognosis?
The prognosis depends on the grade of tumor, its size and location, and the patient’s age and general health as well as the extent of the tumor removed via surgery. For a healthy young person with a slow-growing tumor, the outlook is better; particularly when the growth can be removed entirely. More aggressive tumors can continue to grow if not removed completely. Since each case is unique, this is a question best answered on an individual basis by your neurosurgeon.