Overview of Types of Glioma

Gliomas are the most common type of tumor of the central nervous system (i.e., brain and spinal cord). They originate from glial cells that grow uncontrollably. Based on their microscopic appearance, they can be classified as astrocytomas, ependymomas, and oligodendrogliomas. Glioblastomas (a type of astrocytoma) are the most malignant type.
Considering their growth pattern and infiltrating capacity, gliomas are classified according to the World Health Organization (WHO) by Grades (I-IV). Remarkable progress has introduced molecular and genetic markers to their classification, enabling patients to benefit from prognostic and therapeutic insights. Gliomas can affect patients of all ages, but they are more common in adults.
They can produce symptoms by compression or local invasion of adjacent structures. They can also increase intracranial pressure (pressure within the skull space). A comprehensive evaluation with a detailed history, neurologic exam, and neuroimaging studies is the starting point for managing a suspected glioma patient. Careful patient-centered management with a multidisciplinary approach is recommended.
What Is a Glioma?
To provide a general glioma overview, let’s start by discussing where gliomas originate. These tumors arise from glial cells, which are non-neuronal cells that surround, protect, and support the brain and spinal cord neurons. Gliomas are the most common type of brain tumor (Figure 1). Commonly they appear in older individuals, but they can also affect young patients. The symptoms they produce are related to the invasion or compression of adjacent central nervous system structures or the elevation of intracranial pressure.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
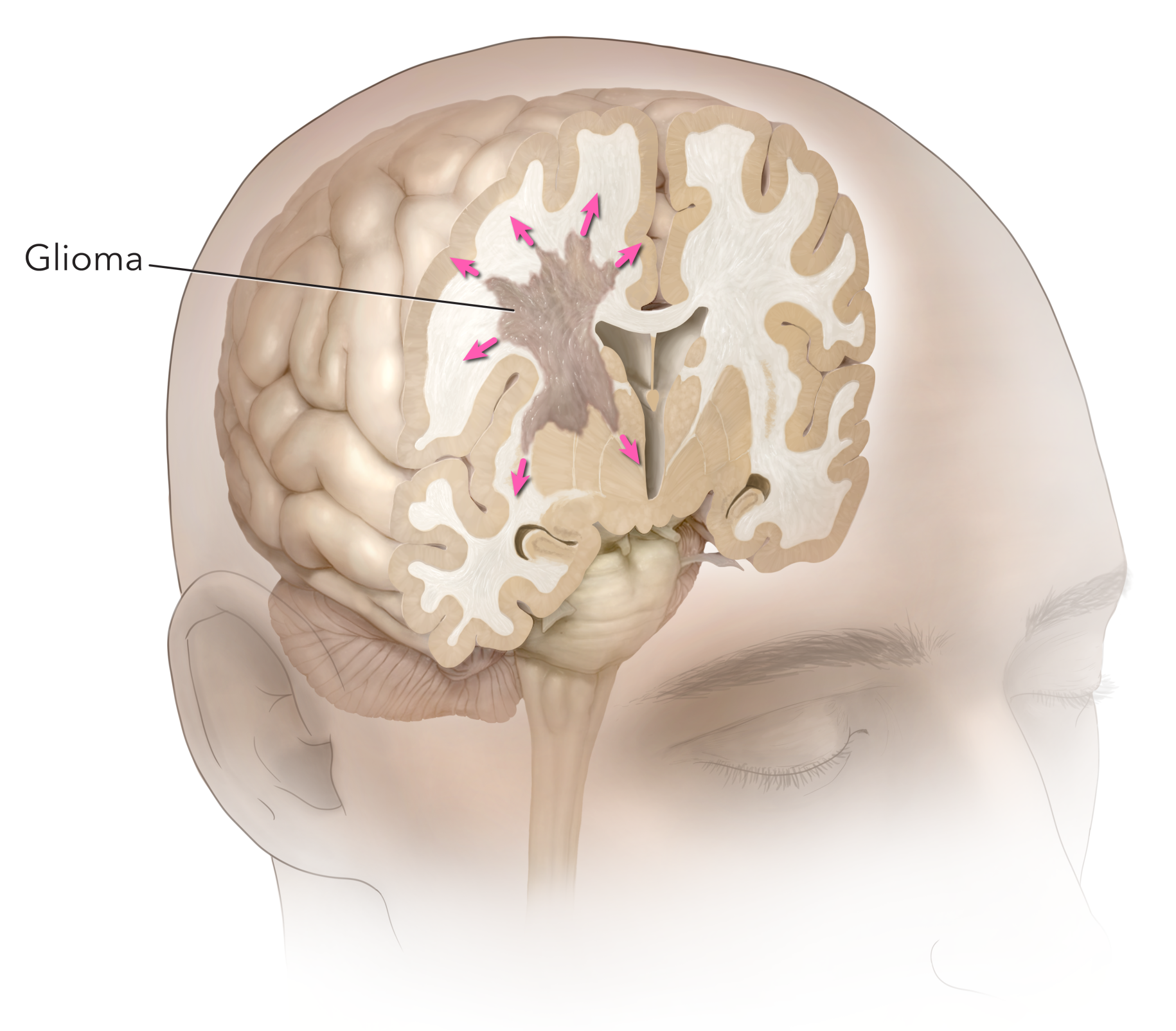
Figure 1: Glioma.
Each year, six out of 100,000 people are diagnosed with gliomas in the United States, and they comprise approximately 33% of all brain tumor diagnoses. Below, we provide an overview of this condition as well as the types of gliomas and their characteristics.
Scientific studies have shown that several risk factors such as age, sex, genetic inheritance, radiation, diet, viral infections, and stress have variable degrees of association with the development of gliomas. However, the exact cause is not known.
There are different subtypes of gliomas, some relatively benign and others malignant. They are classified according to the cells from which they arise (i.e., astrocytes, oligodendrocytes, and ependymal cells). A further classification in WHO Grades I-IV can be done considering the cells architecture. The grade a tumor has is correlated with its aggressiveness.
The management options are observation, surgery, radiation, chemotherapy, or a combination of these. The selection of treatment takes into account baseline patient and tumor characteristics. In general, lower-grade tumors have better outcomes. Therefore, the involvement of a multidisciplinary team that works with the patient to define the best treatment strategy is fundamental.
How Are Gliomas Graded?
The grade of a tumor is determined by the appearance of its cells under microscopic observation. Specific tumor grades can vary by the presence of genetic characteristics. Less invasive and slow-growing tumors have a lower grade and are associated with more prolonged survival.
Grade I tumors occur more commonly in children and teenagers; they are the least invasive and have the highest survival rate. Grade II lesions present initially as slow-growing masses that can progress into higher grades. Grade III tumors are considered malignant; they are more common in adults and have a fast-growing rate. Finally, Grade IV gliomas are the most aggressive, fast-growing, and invasive; they have the worst prognosis.
Low-Grade Glioma
Grade I and Grade II gliomas are considered low-grade gliomas. Commonly they are non-cancerous (i.e., relatively benign) slow-growing tumors that, on rare occasions, can transform into aggressive tumors. They are more common at a younger age, and their symptoms depend on their size and location.
Not all low-grade gliomas have the same origin. For instance, they can be either oligodendrogliomas, astrocytomas, or ependymomas. The type of glial cells from which they arise provides valuable information to define the best treatment option. Prompt diagnosis and treatment improve the patient's prognosis.
High-Grade Glioma
Grade III and Grade IV gliomas are high-grade gliomas. They can appear spontaneously, but, in many cases, they arise from low-grade tumors. Of note, Grade IV lesions are the most aggressive, fast-growing, and invasive. Risk factors associated with their development are the same as for all gliomas. However, the initial alteration that produces the tumor remains unidentified.
Symptoms tend to be more notorious and progressive compared to low-grade gliomas. Headache, seizures, nausea, vomiting, memory difficulty, and confusion are the most common. The basic approach to diagnosis requires a history and physical examination plus associated clinical tests including an MRI.
After a thorough diagnostic process in which a tumor sample is obtained and analyzed by a specialist, the treatment options available are evaluated. The treatment selection is unique to the patient, and the outcomes depend on several factors related to the patient and the tumor. Doctors and scientists continue working to acquire more knowledge and improve patient outcomes via novel treatment options (clinical trials).
Specific Types of Glioma
Besides the grading of gliomas, these tumors can also be classified by the cell type from which they originate. For instance, they can arise from astrocytes, oligodendrocytes, and ependymal cells (Figure 2). Risk factors, symptoms, and diagnosis are non-specific; they follow similar patterns in the different subtypes of gliomas. However, knowing their cell of origin allows the healthcare team to extract meaningful information for identifying specific genetic characteristics that will guide the treatment selection.
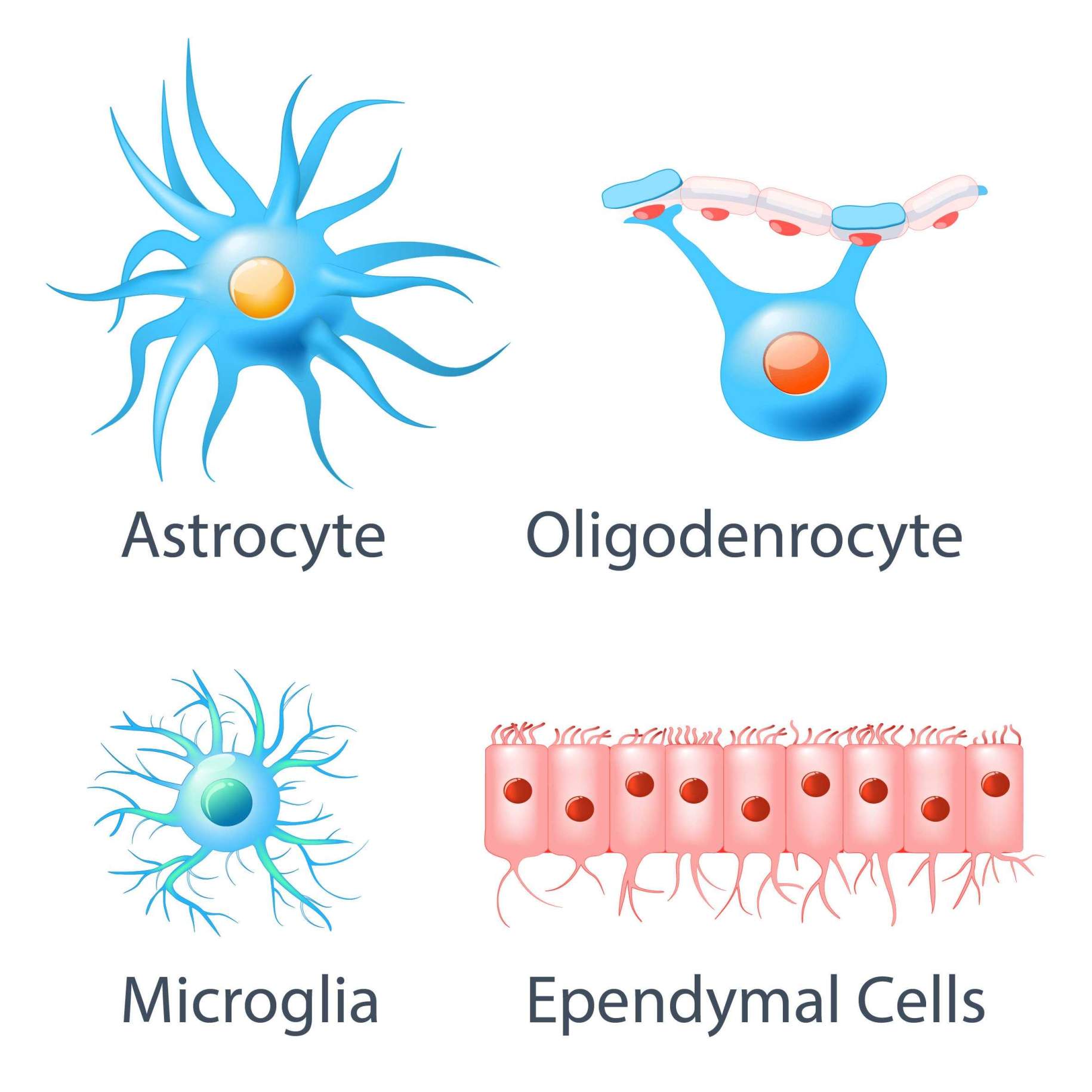
Figure 2: Types of glial cells.
Astrocytoma
Astrocytomas arise from astrocytes. These are star-shaped cells that clean the environment in the brain and support the neurons. Astrocytomas develop when astrocytes grow and divide in a disorderly fashion. They are the most common type of glioma.
There are different subtypes and grades. Grade IV astrocytoma, also referred to as glioblastoma, is the most invasive and aggressive. In general, the treatment modalities are surgery, radiation, and chemotherapy. Low-grade tumors have the best prognosis.
Glioblastoma
Glioblastoma, formerly known as glioblastoma multiforme, is the most common primary brain tumor in adults and is a type of brain cancer. The specific cause for its occurrence is unfortunately not yet identified, but certain genetic conditions and environmental factors increase the risk of development.
Symptoms can be more pronounced due to glioblastomas’ aggressive behavior. They grow fast and infiltrate the healthy, normal brain around them. Their appearance in radiological images is characteristic (Figure 3).
Due to their diffuse growth, complete removal is almost impossible. Both the risk and rate of recurrence are high. If left untreated, the average survival time after diagnosis is 3 to 4 months. Even though the prognosis is unfavorable, there have been reports of long-term survivors. Treatment is unique to the patient through a specialized healthcare team.

Figure 3: Characteristic appearance of a glioblastoma on a magnetic resonance imaging (MRI) scan.
Ependymoma
Ependymomas arise from the cells that line the brain and spinal cord internal fluid (cerebrospinal: CSF) cavities. Ependymal cells produce cerebrospinal fluid. In children, they present mainly in the brain, while in adults, they usually arise in the spinal cord. Some families show clusters of cases which points to a possible genetic association to its occurrence. Treatment modalities are variable and are selected on a case-specific basis. Distinctively, ependymomas have a high sensitivity to radiation therapy. Like the other subtypes, the treatment and prognosis are specific to the patient and the grade of the tumor.
Oligodendroglioma
Oligodendrogliomas arise from oligodendrocytes which are cells that cover the nerve fibers. These cells produce myelin which increases the speed of signal transmission between neurons. For these tumors, the most common presenting symptom is seizures.
In some cases, seizures can affect the patients several years before their diagnosis. They present around 40 years of age. A positive family history doubles the risk of occurrence. Oligodendrogliomas can be either Grade II (low-grade) or Grade III (high-grade). Favorably, survival rates are more than 70% after five years. Treatment depends on the case, but these tumors respond well to chemotherapy.
In summary, gliomas are tumors of the central nervous system that arise from normal glial cells (i.e., astrocytes, oligodendrocytes, and ependymal cells). They are named according to the cells from which they arise. Their classification depends on their shape, growth behavior, and key molecular genetic variations.
The prognosis of gliomas depends on several factors such as age, comorbidities, grade and location of the tumor, response to treatment, and the extent of surgical resection. Patients need to be informed about the importance of close medical follow-up, adherence to the treatment regimen, and lifestyle modifications. A multidisciplinary approach is recommended to enhance patient care and obtain the best possible outcomes.
Get a Second Opinion and Explore Other Treatment Options
Learning that you or a loved one has a glioma can feel overwhelming. After a diagnosis, there are often many questions left unanswered. However, requesting a second opinion may help you or your loved one get peace of mind about the original diagnosis. Importantly, a second opinion may open up other unexplored avenues for treatment.
Dr. Aaron Cohen-Gadol is one of the world’s most prominent neurosurgeons. He specializes in the diagnosis and treatment of various brain tumors, including different types of glioma.
Dr. Cohen-Gahol is renowned for his ability to take on the most challenging surgical cases and his dedication to delivering the best possible patient outcomes. During his extensive career, he has performed over 7,000 complex brain surgeries, mentored hundreds of surgeons and helped give hope to countless patients.
A second opinion from Dr. Cohen-Gadol and his team provides you with an opportunity to get the perspective of a world-renowned neurosurgeon on your diagnosis and treatment plan.
To request a second opinion from Dr. Cohen-Gadol and his team, please fill out the online form.
Key Takeaways
- Gliomas are the most common tumor type of the brain and spinal cord tumor. They arise from glial cells such as astrocytes, oligodendrocytes, and ependymal cells.
- They can be classified by WHO Grades (I-IV) depending on their cell shape, infiltrative capacity, growth rate, and genetic features. High-grade gliomas are the most aggressive. Glioblastoma is the most common primary brain tumor.
- The patient history, physical examination, and clinical tests (i.e., MRI) are fundamental for diagnosis.
- Treatment options are variable and unique to the patient. Therefore, a multidisciplinary approach is recommended for the best patient outcomes.
- Despite scientific advances, high-grade gliomas are very difficult to treat. Therefore, ongoing clinical and basic science investigations are needed to improve the care and outcomes of these patients.











