Overview of Treatment Strategies for Glioma
Glioma treatment is individualized to each patient according to clinical symptoms and imaging findings. It can include surgery, radiation therapy, chemotherapy and medical management, and observation; it often involves a combination of these. The treatment choice can be challenging in cases where the tumor is detected incidentally due to a different condition or when the patient is asymptomatic. Before making the treatment decision, multiple factors such as patient and tumor characteristics are considered.
Surgery to remove the largest amount of tumor safely is the first step in most types of gliomas. Radiation therapy is used following surgery, especially for treating high-grade gliomas. Chemotherapy can be considered in conjunction with other treatment modalities to optimize outcomes. When observation is selected, close follow-up imaging is fundamental. Patients with gliomas greatly benefit from a multidisciplinary team to guide and follow their management.
Surgery
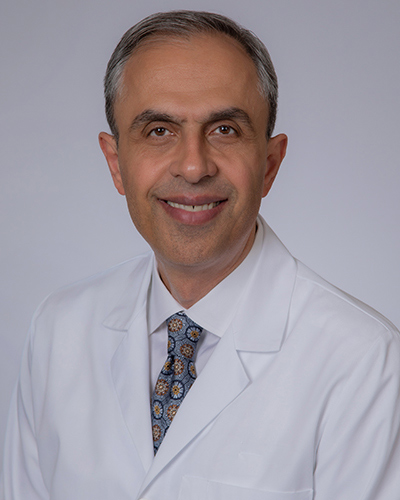
Surgery is the most common initial treatment option in patients with a newly diagnosed glioma (Figure 1). Patients are encouraged to be familiar with their treatment options and the risks/benefits of the surgical approach. A multidisciplinary team of specialists with a history of favorable outcomes is recommended to achieve the best results.
The day of surgery is strategically planned with the involvement of different health care professionals. Each case is unique. Therefore, procedure duration is variable. Surgeries can feel endless for patient family members; nurse circulators offer updates. Surgical complications are uncommon but can happen before, during, or after surgery.
Neurosurgeons receive extensive years of training to be ready to approach any unexpected difficulty. Before the procedure, risks are related to putting the patient to sleep (i.e., anesthesia). Tumor extraction can cause unexpected blood loss and swelling. After surgery, the healthcare team follows and observes the patient to avoid complications during hospitalization.
The quality of life and recovery time is unique to each patient. It can take days to weeks. Return to regular life activities happens in a stepwise fashion but is usually possible within the first 2 months after the operation. Strenuous activities are the last to be incorporated and are typically performed by the third month.
Importantly, gliomas can reoccur and grow back near the site where they originally appeared. Re-growth is more likely in cases where the tumor was not entirely removed during surgery. Long-term side effects of the treatment depend mainly on the size and location of the tumor removal.
Patients can experience emotional, personality, cognitive, and functional changes. The underlying causes of these changes are related to factors such as natural disease progression, surgery, and stress related to postoperative hospitalization. Physical therapy, close medical communication, and adaptation to the living environment are fundamental tools for the long-term management of glioma tumor patients.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Radiation Therapy
Radiation therapy involves using high-energy beams (i.e., external beam radiation) that cause damage and destroy cancer cells (Figure 2). It is performed most commonly after surgery, especially in high-grade glioma cases. In addition, it can be used to treat recurrent gliomas or in gliomas located in high-risk areas of the brain that are not amenable to safe surgical removal.
There are different types of radiation therapies. To treat gliomas, we use 3-D conformal radiation therapy, intensity-modulated radiation therapy and rarely stereotactic radiosurgery. They all follow the same principle of delivering high energy rays of radiation to a precisely defined location. The main variation between them is the size of the beams and the amount of energy delivered. The healthcare team will determine the specific radiation type and frequency of treatment according to the tumor and patient characteristics.

Figure 2: Example of radiation therapy procedure.
Patients can receive a radiation session and go home immediately afterward. Following the procedure, it is safe for the patient to be around other people. The therapy is not painful and takes between a few minutes to an hour. The healthcare team will ensure that the patient is comfortable during the procedure. Post-radiation side effects depend on the dose, schedule, and delivery method.
Initially, weeks following the procedure, patients can feel fatigued and have soreness and/or skin changes near the radiation site. Commonly these initial side effects disappear. However, months after therapy, there can be changes in vision due to clouding of the lens in the eyes, hearing loss, and memory loss.
After completing the radiation therapy, patients are followed by the healthcare team. Gliomas can recur after radiation. Clinical and imaging tests are performed every 3-6 months to monitor progress and ensure early glioma recurrence detection to establish a subsequent treatment plan.
Chemotherapy and Medical Management
Chemotherapy and medical management can be used in conjunction with surgery to treat gliomas. It works by destroying rapidly dividing cells. Tumors are often made up of different types of cells affected differently by specific medications.
Before starting a chemotherapy regimen, patients are evaluated by a multidisciplinary team that will plan a carefully tailored treatment regimen. Chemotherapy medications can be swallowed in pill form or injected into a vein. Treatment regimens vary and often happen in phases with scheduled breaks to allow for patient recovery.
Commonly prescribed chemotherapy medications are temozolomide and bevacizumab. They act by blocking the cell cycle and, therefore, cell growth. Side effects of chemotherapy can be related to the action of the medications or as a result of other treatments. Common short-term side effects include hair loss, nausea, fatigue, nose bleeds, skin rashes, and a weak immune system.
Long-term side effects are variable and depend on several factors. Personality changes and memory loss can happen but are not always associated with the treatment. The healthcare team will walk through the process with the patient to provide all the necessary tools to optimize outcomes. The success of chemotherapy depends on several factors such as the tumor and patient characteristics, the type and length of treatment, and the response to the initial treatments.
Observation
Observation can be considered in cases where the tumor is relatively small and asymptomatic, appearing benign on MRI, or located in areas of high risk where performing surgery can place the vital structures and the patient’s function at risk. When observation is the selected treatment strategy, it is critical to emphasize the importance of regular follow-up visits with serial imaging studies. A biopsy procedure may be needed to confirm the pathology before observation is selected.
Follow-up imaging is recommended at least every 6 or 12 months. If the tumor or symptoms change during follow-ups, the treatment decision will be revisited, and the patient will be offered a new plan. There is no specific type of glioma that is best suited for observation. In general, small low-grade gliomas grow slowly, making them good candidates for observation.
However, high-grade tumors that grow faster can rarely also be managed with observation if there is a significant chance of life-threatening complications related to their surgical removal. Every patient and tumor is unique. The decision to observe or choose a specific treatment paradigm is made while balancing the risks and benefits to maximize the patient’s quality of life.
In summary, there are several treatment options available to manage gliomas. Baseline patient and tumor characteristics are essential starting points for treatment selection. Surgery is the most common initial approach. Radiation therapy follows surgery to optimize tumor control. Chemotherapy is highly specific and can be used in conjunction with other treatments.
Observation and close follow-up can be the best treatment option for rare and specific cases. The treatment of gliomas can be challenging for patients and healthcare providers. Close communication, teamwork, and trust between the patient and the healthcare providers are fundamental to optimizing treatment outcomes.
Key Takeaways
- Treatment of glioma depends on tumor characteristics (i.e., type, size, grade, and location) and the patient’s baseline status (i.e., age, health, and personal preferences).
- In most cases, surgery is the first treatment. However, meaningful tumor removal can be challenging when the tumor is difficult to reach or near vital structures.
- Radiation therapy attempts to control tumor cells with high doses of radiation. It is programmed to precisely target a desired location.
- Chemotherapy can be oral or intravenous. It uses drugs to eliminate tumor cells. The treatment regimen is specific to each tumor.
- Observation requires close clinical and imaging follow-up. If indicated, the treatment plan can be revisited and modified.