Meningioma Surgery

- Evaluation and Observation
- Can All Meningiomas Be Removed?
- Planning and Preparation Before Meningioma Tumor Surgery
- Guidance and Monitoring During Meningioma Surgery
- Types of Meningioma Surgery
- What are the Complications After Meningioma Surgery?
- What are the Side Effects of Meningioma Surgery?
- Life After Meningioma Surgery
- Radiation Therapy
- Rehabilitation Therapy
- How Long Does Meningioma Removal Surgery Take?
- Key Takeaways
- Evaluation and observation
- Can all meningiomas be removed?
- Planning and preparation before surgery
- Guidance and monitoring during surgery
- Types of surgery for meningioma
- Meningioma surgery complications
- Meningioma surgery side effects
- Life after meningioma surgery
- Radiation therapy
- Rehabilitation therapy
Meningioma tumors are the most common type of benign intracranial tumors, making up about a third of all tumors affecting the brain and spinal cord. These tumors are usually benign and grow slowly, but they can endanger critical adjacent structures within the brain and spinal cord.
"Can a meningioma be treated?" is one of the most common questions among patients diagnosed with this tumor. Fortunately, several solutions exist to treat and manage these tumors, including brain meningioma surgery.
Meningioma surgery is the most effective treatment for meningioma, and there are several surgical approaches, depending on the type and location of meningioma. Here is a comprehensive overview of surgical management and treatment strategies for meningiomas.

Evaluation and Observation
Your primary care provider, neurologist, or emergency physician may have found the tumor initially incidentally with cursory imaging (CT scan). A neurosurgeon may recommend more advanced imaging (MRI).
Before I talk about the surgical removal of meningiomas, I want to note that observation is the most common treatment modality for small non-symptomatic meningiomas. Observation entails regular visits (every 6-12 months) to your neurosurgeon for an MRI to make sure the tumor is not growing.
The thought of leaving the tumor alone may be scary, leaving you wondering, "When should a meningioma be removed?" The neurosurgeon may follow up with you routinely, every 6-12 months, and may eventually recommend treatment if the tumor shows evidence of growth or if symptoms develop. Most meningiomas grow very slowly and may go many years without any need for treatment.
I want to emphasize that the diagnosis of a meningioma does not mean a need for surgery and living with a small benign non-symptomatic tumor is very acceptable. There are many people that go about their lives every day who have a small meningioma and do not know about it.
If the tumor is more than 3 cm and symptomatic, surgical resection is advised. Many factors are considered for surgical intervention.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Can All Meningiomas Be Removed?
Before answering this question, it is worth reiterating that not all meningiomas are candidates for surgery. The decision to operate depends on several factors, such as the tumor’s size, location, and growth rate, as well as the patient’s overall health and symptoms.
Moreover, not all meningiomas require immediate removal. Asymptomatic small meningiomas, or those that do not cause symptoms, are often monitored through “watchful waiting.”
Statistics suggest that most meningiomas are resectable, meaning they can be surgically removed. However, some may be deemed not completely removable due to their intricate location, such as being entwined with vital brain structures or blood vessels. This poses a high risk for complications or neurological deficits.
Planning and Preparation Before Meningioma Tumor Surgery
Extensive planning is required when preparing for meningioma surgery to remove a meningioma. Here is an overview of what this phase entails. After you have become a candidate for meningioma tumor surgery, a medical team will evaluate your fitness for anesthesia and surgery (checking your heart and other blood tests are routine).
Planning & Preparation
The planning phase of this process depends on the results of various imaging modalities. MRI and CT scans are often conducted during the evaluation and observation stages.
The results may indicate that the tumor is connected to blood vessels, which sustain its growth. In this case, the surgeon may recommend an angiogram, which is an advanced imaging option that maps out these vessels to determine the layout of the tumor in relation to the blood vessels.
In rare cases, your neurosurgeon may refer you to an interventional radiologist or another neurosurgeon for a procedure where they inject a substance in the vessels immediately near the tumor that blocks the blood supply to the tumor, a process called embolization.This minimizes bleeding during brain meningioma surgery.
Guidance and Monitoring During Meningioma Surgery
Current technology allows for intraoperative image guidance. This technology shows the tumor's exact position under the skull during surgery to remove meningioma in real-time using your specific MRI and CT scans.
Special instruments are used to map the trajectory and direction of the surgery in relation to the tumor and the surgeon’s instruments. The display is shown overhead during surgery.
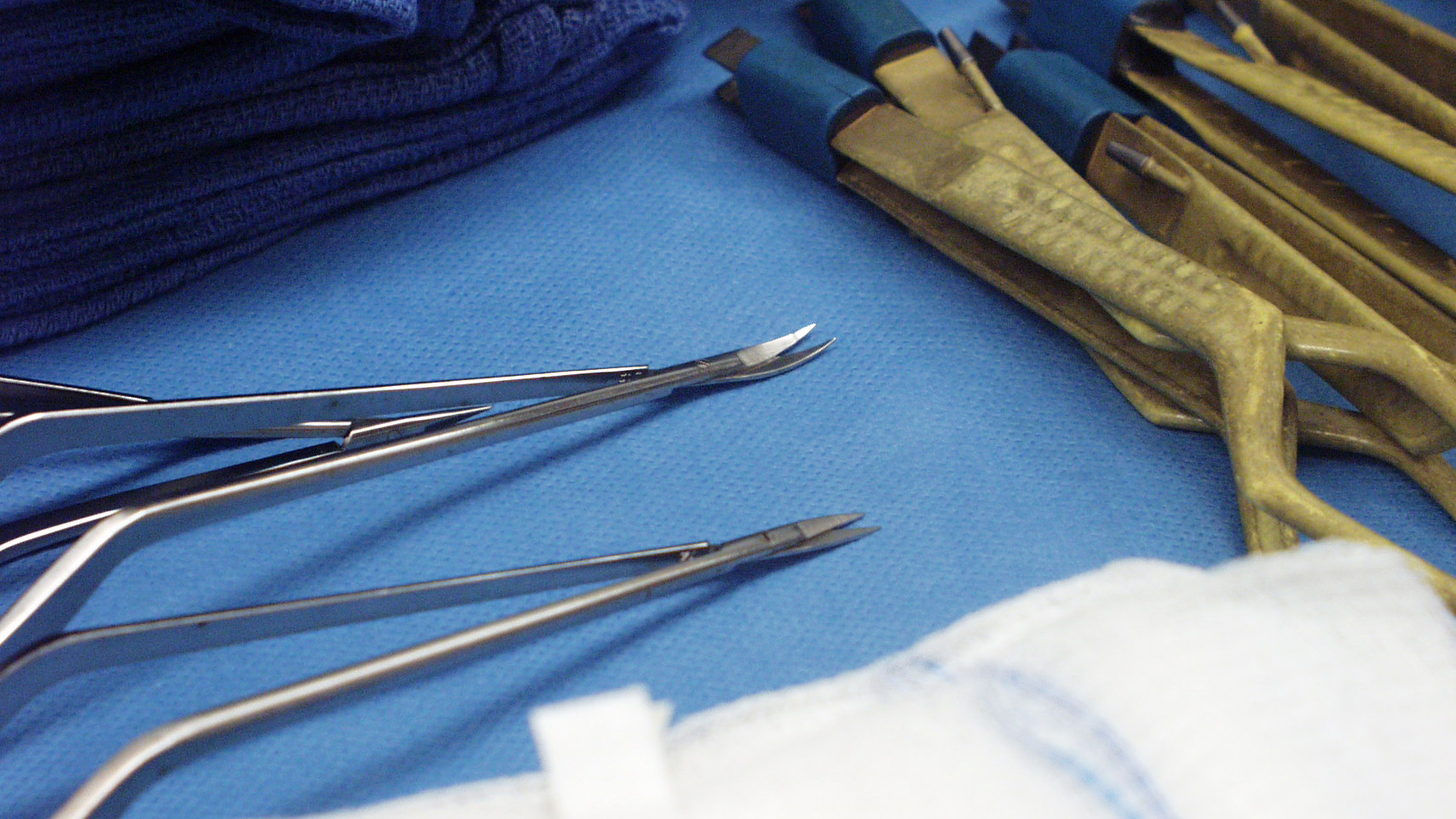
Figure 1. Small scissors (microscissors) are used to remove meningiomas under surgical microscope.
Types of Meningioma Surgery
Surgery or craniotomy is the most effective treatment for meningioma. It entails surgically removing the tumor through various approaches while minimizing damage to the surrounding tissues.
The type of brain meningioma surgery and the specific approach depends on the size and location of the tumor. Here is an overview of the four most common types of surgery used to remove meningiomas.
Craniotomy
A craniotomy is recommended for meningiomas located on the brain's surface or beneath the brain. Some neurosurgeons prefer this technique for almost any location in the brain. It involves removing a small part of the skull to reach the tumor and then closing the opening once the operation is done.

Figure 2. A craniotome is used to create a window (left) to access the underlying tumor capsule (right). The brain-tumor interface is being separated using a microscissor in the right illustration.
Neurosurgeons commonly use a surgical microscope or special eyewear to magnify the tumor and the surrounding parts of the brain. They then use very small surgical tools called micro-instruments to remove as much of the tumor as possible without damaging the surrounding structures.
It is worth noting that this procedure also works for tumors located in other areas, like the base of the skull or near the brainstem.
In this video, Dr. Cohen describes the techniques for surgery to treat a cerebellopontine meningioma.
For more information about the technical aspects of the surgery and extensive experience of Dr. Cohen, please refer to the chapter on Cerebellopontine Meningioma in the Neurosurgical Atlas.
Neuroendoscopic Surgery
Neuroendoscopic surgery may be used for very select tumors located in the inner parts of the brain containing cerebrospinal fluid (lateral ventricles).
This procedure involves making a surgical incision and removing a small window of bone in the skull where an endoscope (small tubular camera) is inserted.
An endoscope is a maneuverable camera with ports for microinstruments. This allows neurosurgeons to access deep and hard-to-reach areas in a minimally invasive way.

Figure 3. An endoscope with its ports is demonstrated.
Many endoscopes are also compatible with neuronavigation (computerized image guidance) to find specific targets within the brain. They use microscopic surgical tools to remove as much of the tumor as safely as possible.
Minimally invasive approaches, such as endoscopy, have less impact on healthy brain. Patients generally experience quicker recovery times.
Endoscopic Endonasal Surgery
Endoscopic endonasal surgery is recommended for some meningiomas located in certain areas at or near the base of the skull. Endoscopic refers to the use of an endoscope and endonasal refers to a surgical approach entering through the nose.
This procedure is also minimally invasive when compared to an open craniotomy. It is primarily performed by neurosurgeons, teamed up with otolaryngologists to help with the endonasal approach.
This procedure involves inserting an endoscope (a long, thin tube fitted with a camera and lighting) through the nose to reach the skull's base. The surgeons then use microscopic surgical tools to remove as much of the tumor as possible through the nasal cavity.
Please note that the ideal procedure is not the one that is minimally invasive but is the one that most safely removes most of the tumor. Therefore, one has to be careful about what procedure is best.
Spinal Surgery
Spinal surgery is recommended for meningiomas growing within the spinal column and compressing the spinal cord, especially if they are causing symptoms. Meningiomas arise from the meninges, which cover the spinal cord.
Tumors may rarely invade nearby bone or grow through the vertebral foramen (natural passageways in the vertebrae where nerves pass). The extent of tumor growth and level of invasion determines the complexity of surgical resection.
If your neurosurgeon feels that removal of your tumor will destabilize the spine, it may be necessary to surgically fuse (reinforce) certain sections of your spine with rods and screws.

What are the Complications After Meningioma Surgery?
Surgery for meningioma is generally safe and effective, but it is important to understand what to expect post-surgery – both the good and the bad.
Like any surgical procedure, it carries potential risks and side effects, such as the following:
Immediate Surgical Risks
Like any major surgery, meningioma removal comes with risks such as infection, bleeding, blood clots, rare stroke or reactions to anesthesia. Your surgical team will monitor you closely for any signs of these complications.
Nerve and Brain Tissue Damage
During surgery, there’s a risk of damage to the surrounding brain tissue and nerves. This could result in various neurological issues, depending on the surgery site, such as weakness, balance problems, or changes in sensation.
Brain Swelling
The brain may swell as a natural response to surgery. Medications are often prescribed to control this swelling, but more invasive measures may be taken in severe cases.
What are the Side Effects of Meningioma Surgery?
Immediately following brain meningioma surgery, you might encounter side effects like headaches, fatigue, and discomfort at the incision site. These are usually temporary and managed with medication.
However, some side effects may last longer or even become permanent. These can include seizures, memory problems, difficulties in concentration, or personality changes. Rehabilitation programs can help some patients recover, function, or adapt to these changes.
Life After Meningioma Surgery
How long can you live after meningioma surgery? How long do you stay in the hospital after meningioma surgery?
What are the side effects of meningioma surgery? These are just some of the many important questions patients have before and after meningioma surgery.
Your stay at the hospital after surgery will range from several days to a week. The first night involves recovery within the ICU environment. After which, you are transferred to the regular floor to mobilize and work with physical therapists. The risks of surgery include temporary worsening of your pre-existing symptoms.
Rare complications can leave you with more weakness and potentially more significant neurological compromises that will delay your return to normal status. In these cases, rehabilitation is especially an important part of your care and recovery.
It is rare to be hospitalized for lengthy periods of time, however, your length of stay is determined by several factors including the extent of the surgical operation and any issues you may have during your hospital stay.
Your neurosurgeon will keep you under close observation during this time to see how your body responds to treatment and recovers from surgery. After your surgery, additional treatments, such as rehabilitation will likely supplement your care.
Your life span after surgery depends on the grade of your tumor and the extent of tumor resection. Most meningiomas are benign and patients enjoy many years of good life after surgery.
Surgery of meningiomas is one of the most satisfying operations for neurosurgeons as they see their patients benefit greatly from their work and continue to see their patients enjoy many years of good life with their families.
Radiation Therapy
While your surgeon will try to remove as much of the tumor without damaging the surrounding healthy tissue as possible, there is always a risk of tumor tissue being left behind.
Radiation therapy may be an option to stop any residual tumor from growing. Radiation therapy uses focused, intense beams of energy to destroy these cells while limiting damage to the surrounding tissue.
Rehabilitation Therapy
Side effects from the natural course of the tumor, and in rare cases your surgery to remove the tumor, may include difficulty speaking, walking, and coordinating physical movements.
Rehabilitation therapy is an important treatment option to help you regain control of these faculties. Early rehabilitation is associated with better overall outcomes.
How Long Does Meningioma Removal Surgery Take?
Meningioma removal surgery can vary in length depending on the size, location, and complexity of the tumor, as well as the patient’s overall health. On average, the procedure typically takes anywhere from 2 to 6 hours. Smaller meningiomas in easily accessible areas of the brain may be removed more quickly, while larger or more complex tumors located near critical blood vessels or nerves often require longer surgical times to ensure safety and precision.
The neurosurgeon must carefully separate the tumor from surrounding brain tissue, which can add time to the operation. In addition to the actual tumor removal, time is also needed for anesthesia, patient preparation, and closure of the surgical site. Although the surgery is lengthy, the goal is to achieve complete or maximum safe removal while minimizing risks. Recovery in the hospital afterward usually involves close monitoring in the intensive care unit for the first 24 to 48 hours.
Key Takeaways
Surgery is an effective treatment option for most meningiomas. Like everything in life, surgery comes with certain risks which are mitigated with careful planning, experience, and follow-through by your neurosurgeon.
It is worth emphasizing that not all meningiomas are the same, and it is advisable to find a talented and experienced neurosurgeon capable of treating and managing your specific type of meningioma.











